Your Starter Guide to Developing a Winning MedTech Software Product
Stay on top of the latest trends in medical technology
Executive summary
Let me begin with my favorite quote that illustrates the state of MedTech today: “The digital health investment climate in one word: Up. Funding, up. Deals, up. Deal sizes, up. Acquisitions, up. Public exits, up.” [Source: Rock Health's report]
A quick look at the latest global medical devices market data confirms that the above is true: the value of the MedTech market stood at $455.34 billion last year, and it’s projected to reach $657.98 billion in 2028.
A combination of factors drives this growth: an increasing focus on early diagnosis and prevention, a rising number of surgical interventions, the rising age-related disease burden (in 2030, the elderly will likely outnumber children under the age of 10), the galloping digitization, and yes—COVID.
My apologies for bringing that topic up, but it’s impossible to disregard the unprecedented impact of the pandemic on healthcare in general and medical technologies in particular. The turmoil of living in lockdown, the medical and psychological effects of social distancing and isolation, and the economic crisis spurred the development of telehealth solutions and mHealth apps enabling safer, distance-based treatment and diagnosis, and the shift towards home care.
When the coronavirus pandemic forced a speedy adoption of digital technologies by all industries, MedTech organizations identified a golden opportunity to boost their bottom line by meeting the urgent demands created by the crisis. If the outbreak taught them one thing, it is that injecting agility into the business model is essential for weathering a storm of the unexpected. By enhancing and diversifying products, digital health pioneers build resilience to thrive in the face of the enduring pandemic and any potential disruptions lurking ahead.
As the momentum for digital health investments is accelerating, savvy MedTech companies are expanding their offering with disruptive technologies like digital health, AI, robotics, and data analytics to build value-added products and fill a niche in the market. Recognizing that now is the time to act, they are eager to leverage the opportunities exposed by COVID-19 through the adoption of intelligent software solutions.
However, many organizations don’t know where to start the transformation. They aren’t sure how to calibrate solutions towards patient-centricity, high usability, and interoperability. Therefore, we’ve created this guide precisely for that group as a good starting point to address the increasingly complex needs of patients, providers, and societies.
Robert Krajewski, Co-Founder & CEO Ideamotive
About this guide
The healthcare industry is on the cusp of a digital transformation that affects all participants, including MedTech companies. Though traditionally, they have developed hardware rather than software, the rules are changing.
As healthcare delivery evolves and digital innovation persists, the boundaries between medical devices and the underlying software are blurring. And the more the industry shifts the balance from treatment to prevention and from physician-centered care toward patient-centered care, the greater the need to incorporate data-driven technologies into medical equipment to empower patients.
We hope this guide will be your introduction to modern MedTech solutions that use cutting-edge software to improve patient wellbeing, enhance diagnostics, and facilitate treatment. Thus, in this publication, we’ll not only discuss medical technology devices but also expand on the digital solutions that underpin them.
Our analysis starts from the definition of MedTech. Next, we look at where to use MedTech products and what medical technologies drive innovation in MedTech. For each, we name a few examples of commercially available products.
Then, we review the current market situation and outlook for the next few years. After that, we investigate crucial technologies behind the development of cutting-edge MedTech software solutions and look at them from the software programming perspective.
Moving on, we examine the benefits of using innovative technologies in healthcare for medical providers and patients and review the main challenges hampering their adoption in the healthcare setting. Finally, we go through the industry’s hot names and glance into the future of MedTech, trying to foresee how it will develop in the next three to five years.
Explore the world of MedTech with us!
GET THE EBOOK VERSION OF THIS GUIDE
We recommend the online guide version for on-screen reading. However, if you’d like to print it out or use it offline, you can get a PDF version here.
By clicking “Get the e-book” you consent to processing your data by Ideamotive Sp. z o. o. for marketing purposes, including email marketing.
Table of Contents
01 MedTech 101: What is MedTech?
Just as you can’t build (a stable) house without a foundation, you shouldn’t be considering launching a MedTech project without understanding the discipline. So before we delve into the intricacies of creating healthcare apps and platforms, let’s set the scene with a quick overview of MedTech and its definitions.
MedTech definition
‘MedTech’ — short for ‘Medical Technology’ — refers to blending technology and medical interventions. The term is very broad, and it encompasses all technologies that diagnose, treat, and improve a person’s health. They may include medical tools, devices, equipment, and software solutions.
When thinking about MedTech, we’ll be talking about things like stethoscopes, thermometers, pregnancy tests, dentures, surgical equipment, and so on, as well as nanomedicine, 3D prints, robotic surgery, and self-diagnosis wearables.
The MedTech Europe association (an organization that represents diagnostic and medical device manufacturers operating in Europe) breaks MedTech down into three main categories:
All three groups are equally important for healthcare and often overlap. However, as we’re a software-oriented company, we’ll dedicate much of our guide specifically to digital solutions, both independent, like Electronic Medical Record and Electronic Health Record (EMR/EHR), patient portals, or mobile health apps, and those powering the other two MedTech product categories.
The diversity of MedTech solutions leaves plenty of room for innovation, which shows in the high number of patents filed. In fact, in 2020, medical technology was the most patented subject matter in the European Patent Office, with 14,295 patent applications.
Where is MedTech used?
When we think about different health care and treatment stages, MedTech solutions can support patients and providers across the entire continuum, from disease and injury prevention to diagnosis and treatment, to health monitoring and post-acute and chronic care.
MedTech market overview
To trace the beginning of digital healthcare technologies, we’d have to go back to the early 1970s, when computed tomography created much excitement among medical professionals. For several years following that invention, digitization in healthcare was associated mainly with the development of digital imaging.
The situation took a new turn once the rise of the internet accelerated breakthroughs in MedTech and digital medicine, connecting patients and doctors and facilitating the collection, analysis, and distribution of health data required to deliver more individualized treatment methods.
But it was the mainstreaming of the internet that represents a quantum leap on the timeline of MedTech evolution. The widespread use of the web unlocked huge advances in custom healthcare software systems and marked the beginning of the digital era that we are living in today.
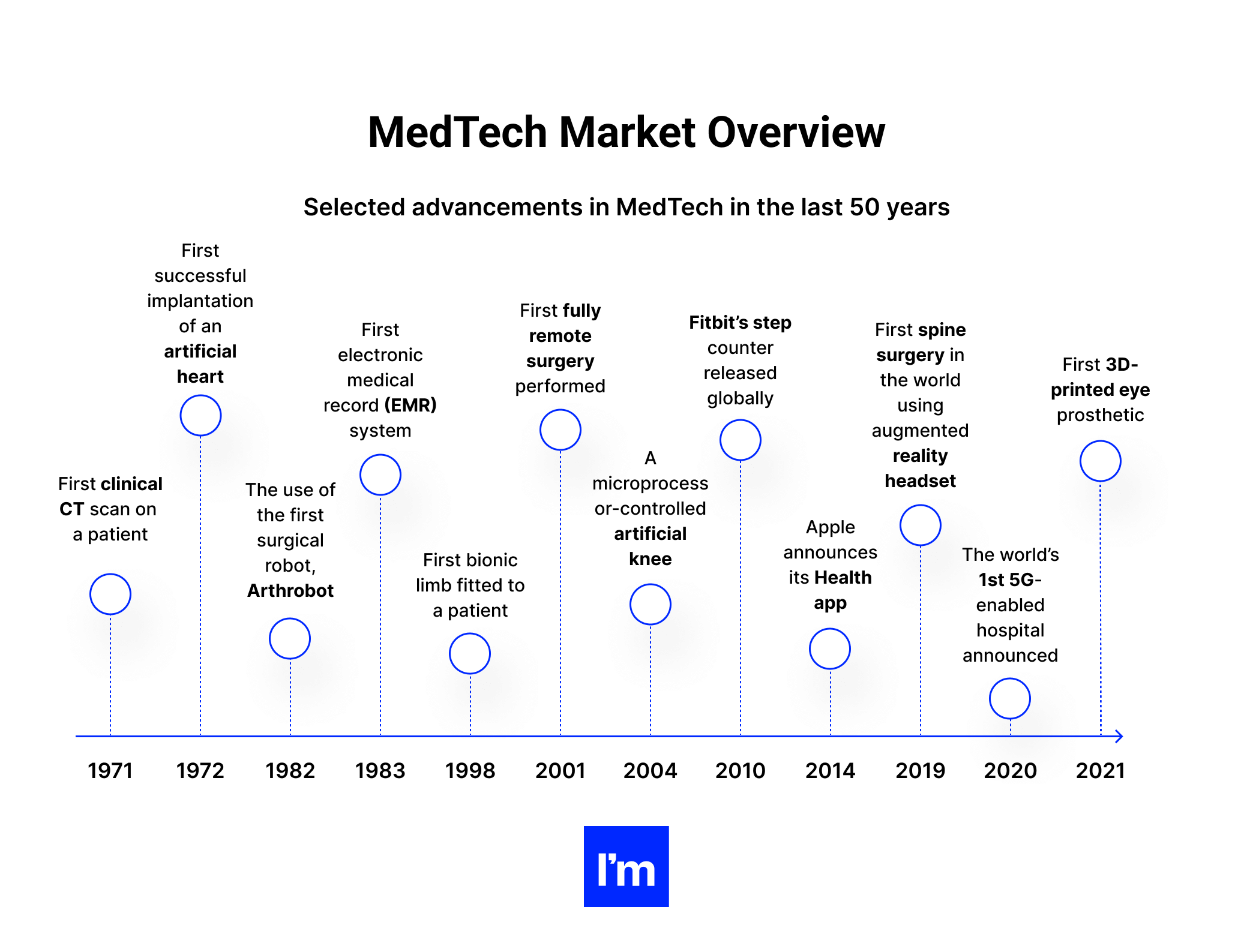
In the last few decades, the rapid pace of technological innovation has spurred a complete transformation of the patient experience—and expectations. As progress in medicine became permanent, and patients gained easier access to their health information through patient portals, wearable devices, mobile health apps, and other inventions, health systems have reoriented toward individualized treatment and empowered individuals. The focus has shifted from ad hoc medical interventions to prevention, patient engagement, and long-term management of chronic conditions.
Implications for healthcare providers:
- Engaging individuals in their wellness and treatment
- Deploying remote and self-care technologies to empower patients
- Ensuring appropriate safeguards to protect patient data
- Training clinicians in the delivery of empathetic and efficient telehealth visits
COVID-19: A new frontier in healthcare
The transformation of healthcare delivery models precedes the pandemic. Nevertheless, the outbreak of COVID-19 catalyzed the adoption of new healthcare and MedTech services, such as telehealth or mHealth apps (mobile health apps), wearables, or remote patient monitoring devices. The necessity to continue healthcare delivery despite disruptions has released pent-up innovations in remote healthcare monitoring, management, and delivery.
Patients who might have been reluctant to accept telehealth solutions earlier had no choice but to embrace them amid lockdowns and growing concerns over exposure to the virus (preventing the spread of COVID-19 was the reason for choosing eHealth technologies for 70% of individuals). Virtual tools and MedTech cloud-based software systems became essential for communication with doctors for many patients in isolation.
A recent study by Accenture found that nearly half of surveyed patients from the USA, UK, France, Germany, China, and Japan are currently getting treatment at home instead of visiting their healthcare providers. About 37% of individuals use video conference calls to talk to their doctors, 36% go to online chat, and 31% communicate via a mobile app.
But perhaps the most critical findings guiding the developments in digital healthcare solutions are the fact that 60% of patients plan to use technology, even more, to get in touch with healthcare providers. In addition, 78% of respondents in another survey said they were satisfied with their telehealth experience.
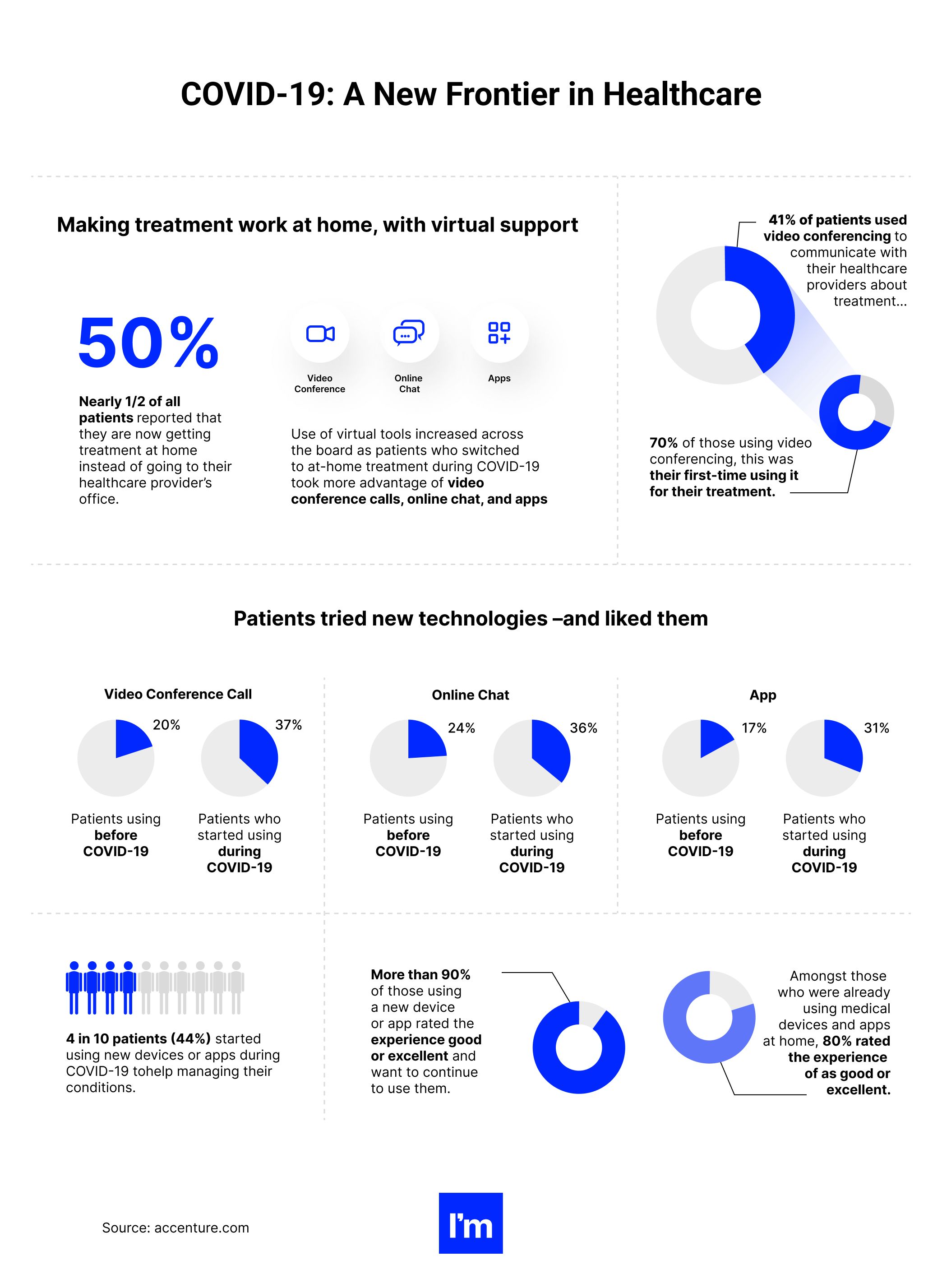
Telemedicine has emerged as a frontline technology during the pandemic, clearing the way to adopt other digital-based healthcare innovations. For example, wearable healthcare devices have experienced a surge of popularity, as they facilitate health monitoring without the need to leave home. Before the pandemic erupted, the global wearable medical device market was already worth $29.76 billion. By 2027, analysts expect it to reach $195.57 billion, growing at a CAGR of 26.4% during the forecast period.
Another interesting trend that we have seen developing in the aftermath of the pandemic is extending virtual technologies to clinical trials. Especially the fact that 75% of participants were considering dropping out of their trial programs during the pandemic.
Specialists have determined that bringing clinical trials to patient homes may be particularly effective in the case of individuals with neurological conditions or impaired mobility who may experience difficulties accessing healthcare facilities in the course of ‘standard’ trials.
Finally, as we discuss the relationship between digital medical technologies and pandemics, we must mention digital epidemiological surveillance technology. The term refers to the aggregation and analysis of health-related data (official and self-reported) and other information sourced from news sites, GPS systems, social networks, web searches, etc., to track the spread of infection.
Like telehealth solutions or mobile apps, digital surveillance dashboards and apps have been in use for quite some time already. For example, a similar health security system was used over a decade ago in Canada and the United States to determine influenza incidence based on search engine entries.
Likewise, the WHO and state governments regularly use HealthMap, a global disease monitoring system, to capture digital clues about disease outbreaks based on online activity analysis. However, considering the unprecedented scope of the COVID-19 pandemic, the role of technology solutions used for preventing, managing, and reducing the toll of this and any future outbreaks will likely grow.
Facts & figures: The global medical device industry market
- The USA is the largest MedTech market, with 41.6% of the global share, according to MedTech Europe.
- Throughout the 2021-2028 period, the US MedTech market is projected to grow at a CAGR of 5.4%, to reach nearly $658 billion.
- In 2020, the European medical technology market was estimated at roughly €140 billion (over $158 billion), making it the second-largest MedTech market globally.
- In the same year, the venture capital investment in MedTech companies amounted to $6.6 billion across the two leading markets.
- Inside Europe, Germany, France, and Italy are the biggest markets for MedTech. Other countries with a considerable share in the European market include Poland, Switzerland, and the UK.
- It’s estimated that there are more than 33,000 medical technology companies in Europe alone, providing jobs to over 760,000 people.
- In 2020, medical technology was the most patented subject matter at the European Patent Office, with 14,295 applications, a rise of 2.6% from 2019.
- In the USA, there are nearly 15,000 MedTech establishments. They jointly employ 397,000 people. Indirectly, the industry is responsible for creating almost 2 million jobs.
02 The latest technology disruptions in digital health
As the digital revolution continues to transform healthcare, let's dive into the cutting-edge technology reshaping the landscape.
At the forefront of this disruption is the adoption of Electronic Health Record (EHR) software, like MEDITECH EHR, which has transformed how medical records are managed and shared. MEDITECH hospital software not only streamlines workflows but also enhances patient care by providing critical data at the fingertips of healthcare professionals.
Beyond EHR systems, we are also seeing a rise in medical device management software and quality management software for medical devices, such as Greenlight Guru quality management software. These tools are empowering medical device companies to meet stringent regulatory requirements while ensuring the highest standards of quality and safety.
Simultaneously, the importance of compliance in healthcare has given birth to advanced regulatory management software and regulatory software solutions. Rimsys Regulatory Management Software, for instance, automates and streamlines regulatory processes, ensuring compliance while reducing complexity.
Further advancements are also being made in medical device QMS software and health information technology software, transforming how information is processed, stored, and shared within the healthcare sector.
In addition to hospital EHR software, Electronic Medical Record (EMR) software, including MEDITECH's EMR solutions, are also contributing to the transformation. These systems are revolutionizing how healthcare data is recorded, stored, and accessed, making patient care more efficient and effective.
In summary, the latest disruptions in digital health, from EHR and EMR healthcare software to advanced regulatory affairs software, are revolutionizing the medical industry. As we step into the future, these technologies promise to make healthcare more efficient, effective, and patient-focused.
It wasn’t until the 19th century that medicine as we know it today began. The Industrial Revolution brought a valuable contribution to its development as a discipline. The rise of scientific discoveries led to numerous advances in medical devices and instruments.
The Age of Industry saw the creation of medical equipment like the stethoscope, ophthalmoscope, x-ray technology, and corrective eyeglasses. Doctors performed the first surgical operation using diethyl ether as an anesthetic, and researchers formulated the principles for the development of EEG.
However, the earliest predecessors of today’s medical devices date back to ancient times. For example, archeologists identified a rich collection of surgical instruments, including bone levers, vaginal and rectal specula, and a portable probe case among the artifacts recovered from an excavation site at Pompeii. The first prosthetic devices go back even earlier—possibly as far as 1069 BC.
These past breakthroughs are as exciting as the latest MedTech innovations powered by data analytics, sophisticated algorithms, and elaborate software systems. We’ll review some of them in this section.
IoT devices, biosensors, and trackers
Let’s start with solutions that have seen tremendous growth in demand in the last few years. The Internet of Things devices (electronic devices interconnected via wireless protocols such as Bluetooth, Wi-Fi, NFC, or—more recently—5G) have become ubiquitous in manufacturing, utilities, transportation, retail, FinTech, and consumer electronics.
According to estimates, there are over 10 billion active IoT devices worldwide. In the next decade, that number is expected to surpass 25 billion, or even reach twice that amount, as stated in other evaluations.
The first connected devices appeared at the dawn of the 1990s. But the term ‘The Internet of Things’ wasn’t coined until the end of the decade. The earliest IoT inventions were mostly household items, such as a toaster or the coffee machine. As these solutions were gaining ground, smart devices started to make their way into the healthcare industry.
One of the essential roles smart devices play in healthcare is enabling remote patient monitoring and care. This capability proved invaluable amid COVID-19 lockdowns and social distancing measures, but the IoT technology is extremely useful for patients and healthcare providers in other contexts, too. Here are some examples of the Internet of Things in use in medicine and healthcare:
- By collecting vitals from smart sensors and sending them in near real-time over the internet, connected solutions help doctors monitor patients with chronic illnesses like diabetes, heart and respiratory conditions, or asthma.
- Wearable trackers help better manage the health of some cancer patients, providing data that complements the patient's self-reported symptoms.
- The latest IoT developments focus on solving the issue of drug non-adherence with connected pills.
- Healthcare providers increasingly use IoT-based location services for tracking assets and personnel around medical facilities to streamline operations and provide more effective services.
- It may seem that hand hygiene has improved due to the pandemic, with more people recognizing the need to wash their hands longer and more thoroughly. However, research shows that even in the face of the COVID-19 threat, 1 in 4 Americans don’t wash their hands regularly. Similarly astounding results were reported by the UK researchers who found that only 40% of the respondents always remember to wash their hands after sneezing, coughing, or blowing their nose. IoT also has an answer for that. Connected hand-hygiene stations already help monitor hand hygiene compliance in hospital facilities, and their application could now also be extended to patients.
- On the whole, IoT technology serves as an enabler for the expanding field of personalized medicine, which allows for tailoring treatment methods to a specific individual.
Business potential
The benefits of IoT solutions for medical care are hard to ignore. By providing vital health information in real-time, wearables and other connected devices allow patients to take care of their wellbeing and immediately seek assistance when needed. They also increase patient engagement, equipping providers with more relevant data to make quicker, more accurate diagnoses.
Empowering facility managers with data collected from IoT sensors enables streamlined hospital operations and more effective use of medical equipment. In addition, making essential information readily available for hospital staff and improving communication between personnel also positively impacts the overall patient experience.
Even more importantly, by unlocking faster and more precise health information, IoT devices can help speed up diagnoses and examination, which, on the global scale, leads to shorter wait times through more effective visits. Going one step further, a body of research exists suggesting that data-driven technologies can also cut down the length of hospitalization. Advamed estimated, for example, that the use of advanced medical technology helps reduce the duration of hospital stays by 58 percent.
Considering these and other benefits of IoT and smart sensors for patients, hospitals, and medical providers, it’s not surprising that the healthcare IoT market is booming. Currently worth a little under $72 billion, it is expected to reach over $446.5 billion by 2028, growing at a massive CAGR of nearly 26 percent.
Among the key drivers nurturing that growth, we find the maturity of IoT solutions and their successful implementations in healthcare and other industries, the surge in remote medicine triggered by the pandemic, and the increasing awareness of the significance of patient engagement in their health.
Types of IoT-driven healthcare products
- Medical devices: infusion pumps, ventilators, incubators, telemetry, smart stethoscopes, medical imaging, ECG, heart rate monitors, spirometers, oximetry, ventilators, capnography monitors, depth of consciousness monitors, bio patch technology, respiratory rate trackers
- Remote and chronic disease management: remote medical assistance, fit trackers, bio patches, smartwatches, smart glucose monitoring, pacemakers, defibrillators, neurostimulators, implantable device monitoring, remote terminal units
- Asset monitoring: real-time tracking of wheelchairs, infusion pumps, medication carts, etc.
- Other: personnel tracking, patient wandering systems, smart beds, fall detection, smart pill
Barriers to adoption
Even though IoT devices are now a part of everyday life, healthcare providers have traditionally been slow on their uptake for several reasons. Among them, data privacy concerns are the major hurdle impeding the speedy adoption of smart solutions in hospitals and medical practices.
Many patients still take issue with sharing sensitive health data, fearing breaches and misuse. And as reports suggest, their qualms are not entirely unfounded—in the USA alone, more than 40 million patient records were compromised in 2021.
Underlying software
Upon hearing the term ‘the Internet of Things,’ many think primarily of hardware. However, it’s impossible to collect data from sensors and communicate between connected devices without specialized IoT software.
IoT systems and applications perform two core functions. First, they provide connectivity using wired or wireless technologies (Bluetooth, radio connectivity, 5G, Ethernet, etc.). Secondly, they automate the entire process of data collection, transfer, analysis, and autonomous response. Advanced solutions often have AI and big data management and analytics components embedded.
Examples of existing solutions
- Abilify MyCite - A smart pill for treating schizophrenia and bipolar I disorder with an embedded sensor that tracks whether the user took their medicine. Abilify MyCite
- TTP’s smart surgical nail - A robust smart device implanted in a fractured bone to monitor the healing. Smart surgical nail
- InPen - An insulin pen that offers dose calculations and updates through a mobile app. InPen
3D printing
The concept of 3D printing emerged in the middle of the 20th century. But it wasn’t until 1984 when Chuck Hull filed for a patent for ‘a system for generating three-dimensional objects.’ As a result, technology began entering the mainstream in the mid-2000s.
3D printing originated in the manufacturing industry, but healthcare was among the early adopters. First, dental implants and prosthetic equipment emerged in the late 1990s and early 2000s. Since then, the capabilities of the technology have evolved immensely, and there are virtually no limits to its use.
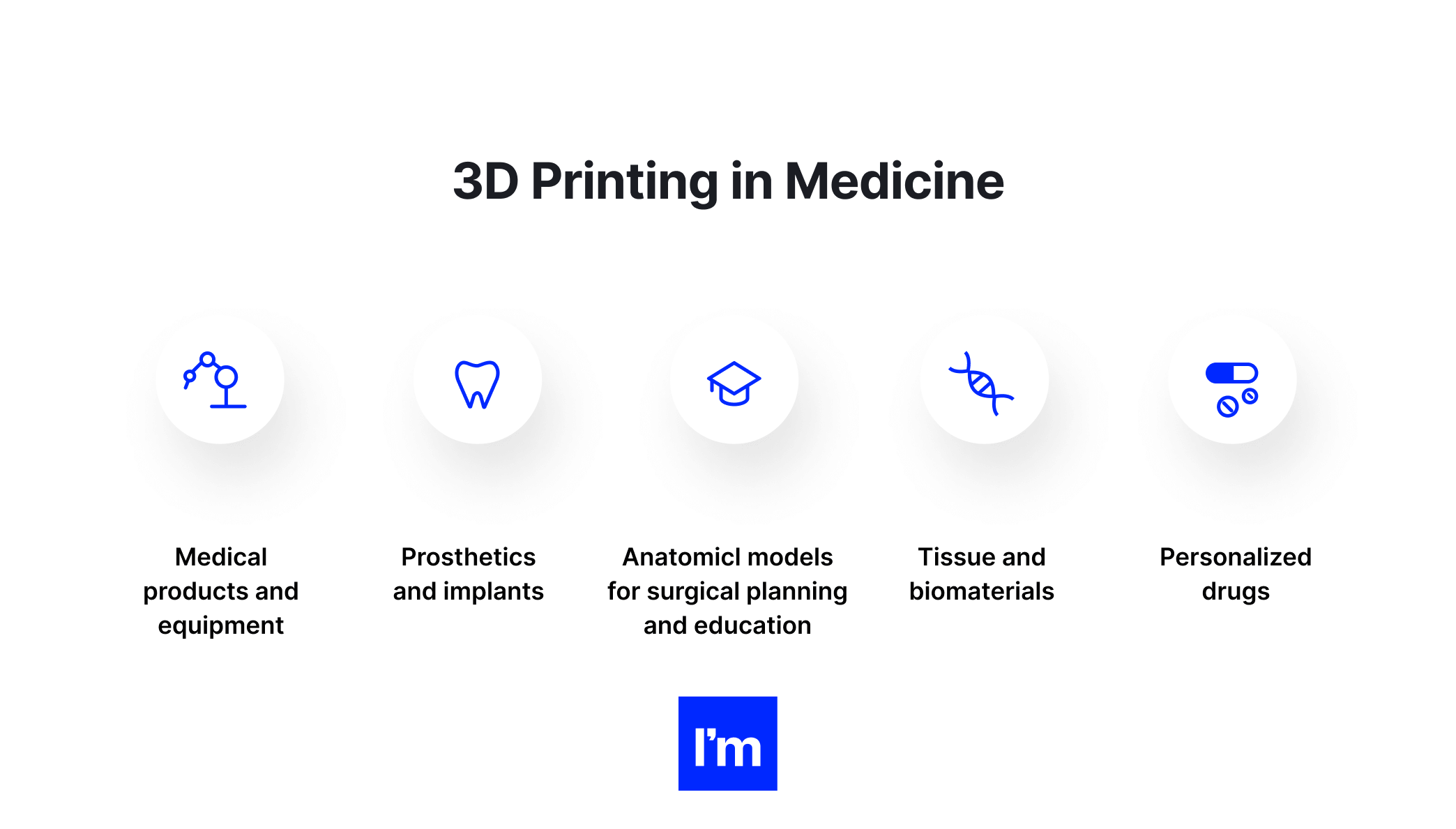
Today, 3D printing has medical applications in the following areas, as defined by the US Food and Drug Administration:
- Medical equipment: including surgical devices such as forceps, retractors, and medical clamps, orthopedic and cranial implants, prosthetics, and dental restorations.
- Biologics: such as synthetic bones and 3D-printed organs and tissues used for clinical research.
- Drugs: 3D printers allow printing multiple drugs in a single pill and create new opportunities for fast production of personalized medication.
Business potential
3D printing is one of the most disruptive technologies poised to make healthcare affordable, readily accessible, and personalized in the medical field. Notwithstanding exciting breakthroughs in the area over the last 20 years, the technology continues to advance, and its immense potential remains largely untapped, especially in the production of biomaterials and drugs.
Regarding the increasing interest in personalized medicine, 3D printing is set for explosive growth, which shows in market studies. Namely, the 3D printing of medical devices is expected to reach $5.1 billion within the next five years, growing at a CAGR of 16.3 percent.
The market's growth continues despite the hardships of the COVID-19 pandemic, which disrupted global supply chains and redirected the focus of hospitals and researchers to battling the coronavirus. Moreover, as the range of raw materials for printing is widening and process and printer innovations evolve, they are paving the way for 3D printing to enable democratized healthcare.
Barriers to entry
One of the key barriers that affect the pace of adoption of 3D printing is the scarcity of a trained workforce. At various stages of production, the skills required to operate printers and handle the printouts include software engineering, design capabilities, as well as data preparation, quality assurance, and machine operation skills.
Some software companies claim that healthcare providers with no experience in 3D printing can use their systems without support from a professional. However, it is highly unlikely that they will be able to create accurate and safe 3D models without trained specialists.
Underlying software
The 3D printing technology comes with a software suite for 3D modeling and printing. The entire process of generating a 3D object starts with creating a model in a modeling program. The program typically covers such stages of 3D creation as modeling, animation, and simulation.
While there is a broad selection of 3D modeling software available on the market, including open source tools, making a choice that matches your use case is critical for generating fully-functional 3D printouts. The available programs vary greatly in their use and features. For example, some are well suited to creating basic shapes, while others serve specialized uses, such as ballistic analyses, architectural components, or medical equipment.
Apart from the modeling tool, a separate platform is usually needed to slice a ready model and prepare it for printing. You might also need a dedicated app to operate the printing devices remotely.
Examples of existing solutions
- A 3D-printed eye - In November 2021, surgeons from Moorfields Eye Hospital in London fitted one of their patients with the world's first fully digital 3D printed prosthetic eye developed by researchers from Fraunhofer IGD. Fraunhofer Technology
- 3D-printed pills - The world’s first 3D-printed prescription medicine was approved in 2015 by FDA to treat seizures in epilepsy patients. Spritam
- Dental 3D printing - A printer for dental professionals to create dental crowns, bridges, and interim dentures. SprintRay
Next-generation sequencing
Next-generation sequencing (NGS) refers to the application of massively parallel genetic sequencing technology to study genetic variations of DNA and RNA. As opposed to conventional methods, NGS allows the sequencing of millions of DNA fragments simultaneously instead of one at a time. The technology's high throughput, accuracy, and speed makes it the best tool for identifying at-risk populations and targeted therapies.
Although NGS entered commercial use in the early 2000s, its primary applications have largely comprised genome research and applied sciences. In addition, NGS often serves as a screening tool for foodborne pathogens in routine clinical practice.
The outbreak of COVID-19 has brought to light the utility of NGS in epidemiology. The technology allowed researchers to study the virus spread and evolution essential to steering the global response to the pandemic. Next-generation sequencing has also proved efficient in rapid and large-scale COVID-19 diagnostics. As the widespread adoption of NGS is gaining momentum, medical professionals will likely use the technology increasingly often in routine clinical practice.
Business potential
By 2030, the global NGS market size will reach $35.5 million, up from nearly 6.6 million in 2020. The growth is majorly due to a surge in demand for genome mapping, a growing number of technology applications, and increased spending on healthcare. The widening adoption of cloud-based infrastructure and growing data also play a part.
The major areas for NGS application include:
- Epidemiological analysis
- Personalized precision medicine
- Hereditary cancer testing
- Targeted therapy
Barriers to adoption
As a data-intensive research method, NGS requires advanced IT infrastructure. In addition, test results are typically interpreted by a molecular pathologist or a bioinformatics specialist, making next-generation sequencing a technology that involves specific expertise.
However, emerging software solutions allow users without programming skills to run the sequencing reliably and consistently. And with the fast progress of IT technologies, advanced hardware, software, and the underlying network are becoming more and more accessible for healthcare organizations.
Underlying software
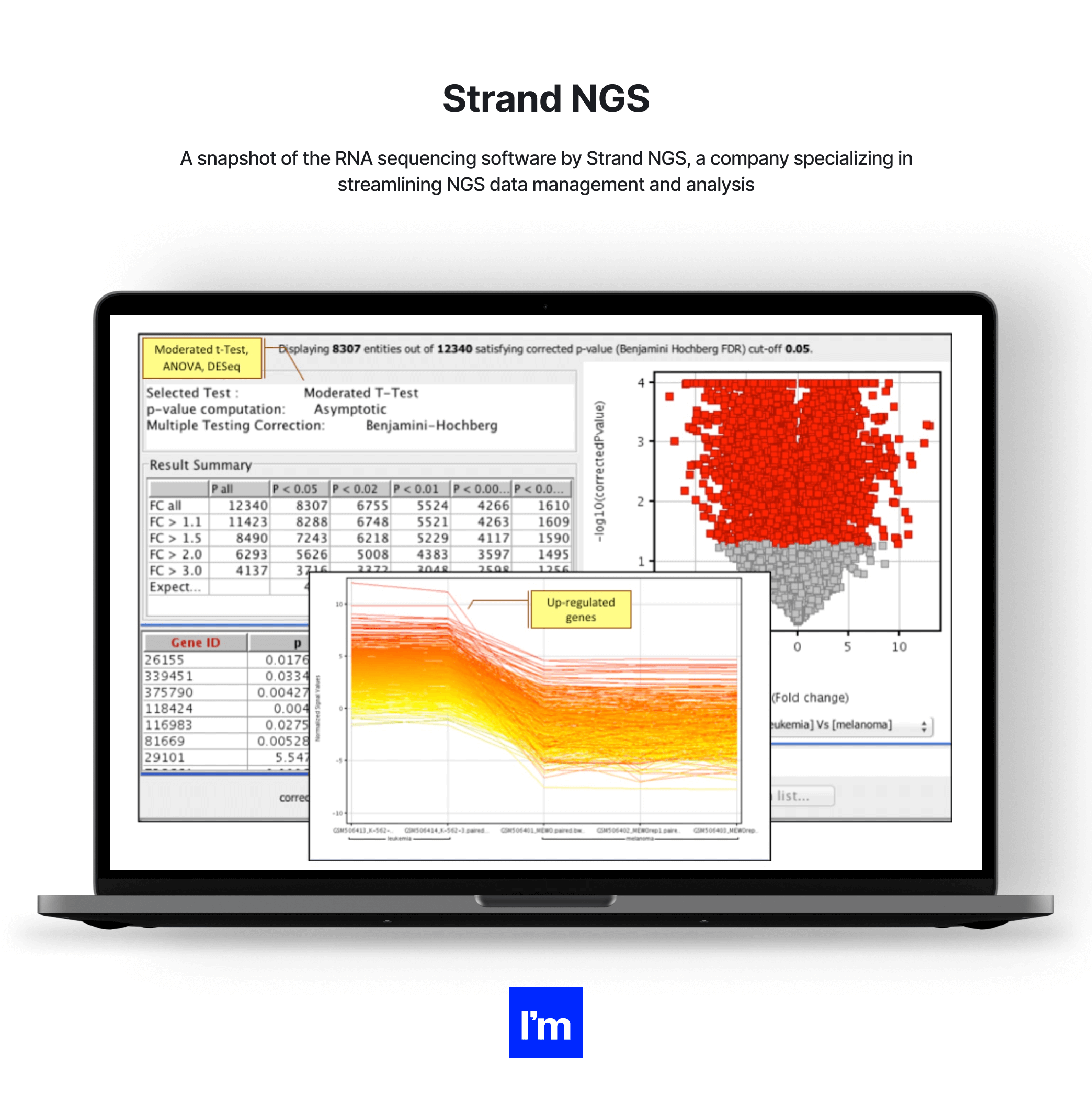
Because of the volume and complexity of NGS data, processing and analyzing it is extremely challenging. Therefore, the technology requires an advanced software framework to efficiently manage NGS workflows.
At its core, the NGS database software must provide data analysis, browsing, filtering, reporting, visualization, and alignment. It can also incorporate features such as managing disease-specific information or generating data-based predictions.
Examples of existing solutions
- Ion Torrent - A rapid and compact NGS technology that offers custom workflows that personnel can supposedly use without specialized training in bioinformatics. Ion Torrent
- Strand NGS - An integrated platform providing analysis, management, and visualization tools for NGS data. Strand NGS
- Illumina - A portfolio of benchtop and production-scale sequencing platforms. Illumina
How are AI, machine learning, and data science changing the healthcare game?
Whether we are talking about IoT healthcare devices, 3D printing solutions, or mHealth apps, modern technology-enabled healthcare would not exist without machine intelligence and data science developments. By imitating human abilities without the limitations of energy, power, and time, they play a crucial role in delivering effective, efficient, and personalized healthcare today.
Like other technologies underlying cutting-edge medical devices and software platforms, AI, ML, and data science have been around for some time, but their adoption soared during the coronavirus pandemic. To contain the virus and unburden healthcare systems globally, medical and healthcare organizations well-versed in forefront tech were developing new AI models to enhance all aspects of patient care and harnessing data to improve and accelerate decision-making.
As a result, in 2021, 42 percent of healthcare organizations already had AI models in production (from the early stage to the sophisticated level), while 34 percent evaluated AI use cases or developed pilot models. When we look at healthcare analytics, nearly 80 percent of healthcare leaders and professionals plan to maintain the investments in data analytics made during the pandemic long term.
Not sure how machine learning differs from AI, data mining, and analytics?
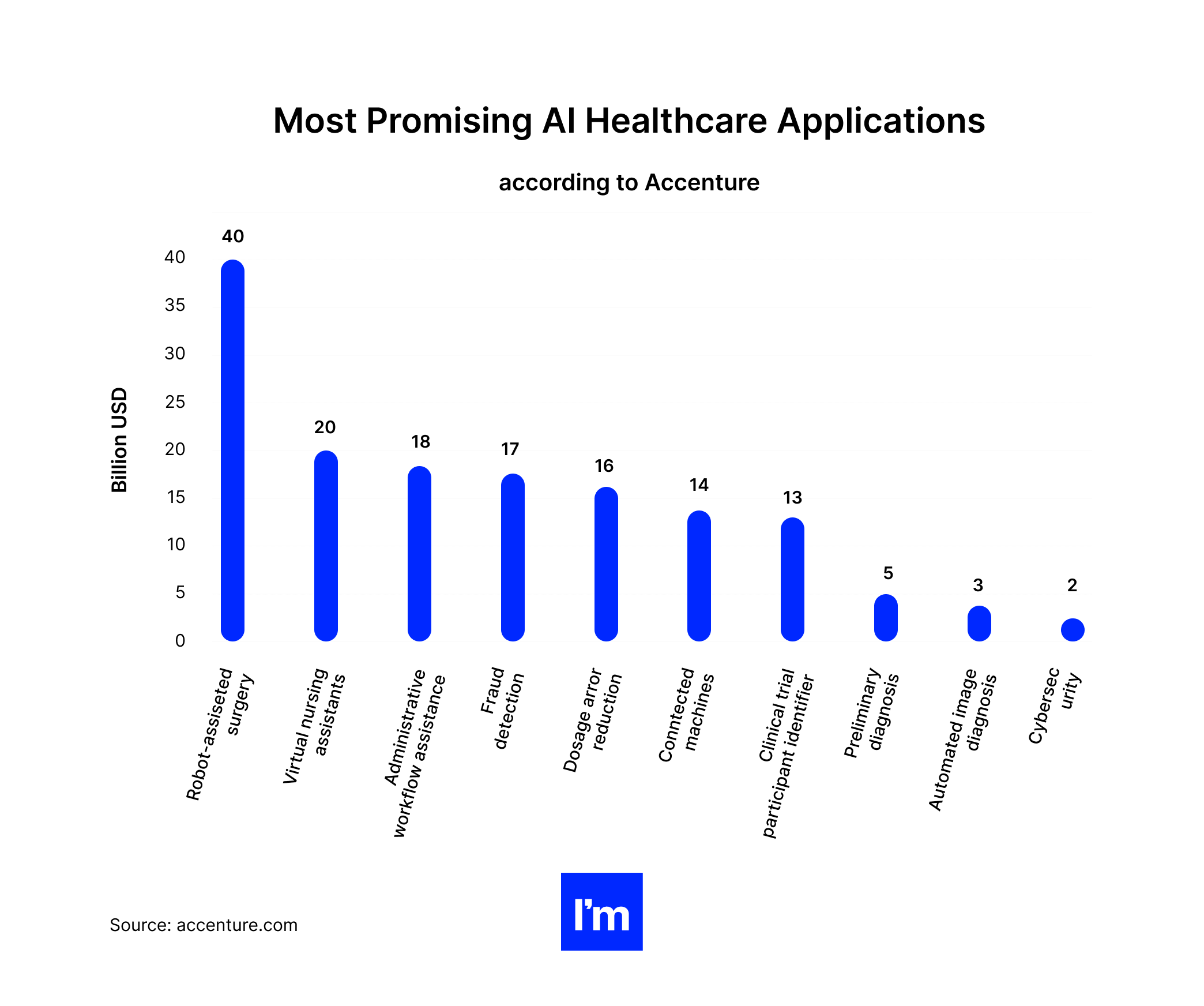
The role of big data analytics and AI in MedTech and healthcare
The scope of AI, machine learning, and data analytics in healthcare (and, more specifically, in MedTech and digital medicine solutions) is so broad that it deserves a guide of its own. Therefore, we will cover several areas where we foresee the greatest potential for medicine and wellness, as presenting all of the uses for data and AI in MedTech and digital health is impossible.
Improving diagnostic accuracy and speed
It’s no secret that a delayed diagnosis directly impacts the duration and chances of recovery. For example, BMJ reports that a delay of even one month for cancer patients increases the risk of death by 6-13 percent. According to the same source, a surgical delay of 12 weeks for all patients with breast cancer would lead to 1,400 excess deaths in the UK and 6,100 in the USA. Meanwhile, in the case of some rare chronic diseases, the average time for diagnosis in the USA is… 7.6 years!
The delays stem from various issues: insufficient information on rare symptoms or diseases, inaccurate patient interview data, and the lack of appropriate diagnostic devices in a given facility or hospital. Providers can resolve some of these issues by integrating AI-driven devices and hardware into their system and training machine algorithms to detect anomalies accurately and analyze thousands of results rapidly.
Indeed, a significant body of research shows that algorithms are at least as efficient and accurate as health professionals in delivering a medical diagnosis. With nearly half of the world having no access to healthcare specialists, AI solutions (such as chatbots used for preliminary diagnosis or portable devices capable of detecting biomarkers) could be a major improvement in leveling the distribution of healthcare and making it more affordable.
Predicting epidemic conditions
AI and data analytics also have an interesting and promising use in epidemiology. By working with huge sets of data, such as population density, mobility patterns, reported cases, weather reports, etc., predictive analytics solutions can play a significant role in predicting an outbreak of contagious diseases like COVID-19 on a large scale.
Given that appropriate data feeds into the algorithm, AI coupled with a predictive engine can also identify population patterns that indicate a high risk of developing diseases, such as diabetes, asthma, or heart disease in a given population.
The systems may pull data for predictions from databases, third-party suppliers, social media, browser searches, and individual IoT-enabled medical devices like smart thermometers or health trackers. Meanwhile, updates about the current state of epidemiology and reports on symptoms can appear in a mobile app.
Eliminating staff burnout
Ninety-two percent of clinicians report that excess administrative tasks contributed to their burnout. These findings are particularly alarming as healthcare worker burnout rates have increased from 50 to 70 percent amid the COVID-19 pandemic. Of course, other issues add to this grave situation, including overdrawn shifts, staff shortages, and excessive staffing ratios. Nevertheless, too much time spent on repetitive office tasks instead of caring for patients makes clinicians feel detached from their work and makes them question their life choices.
Artificial intelligence-driven tools provide solutions that can relieve individual professionals through automation. For example, transferring time-consuming and low-value work to machines frees doctors’ and nurses’ time and lets them focus on patient-facing activities. Additionally, empowering patients with AI-based devices to self-service their care needs further decreases the amount of work on the clinicians’ end. As a result, healthcare leaders expect their staff to gain back at least 90 minutes per day when they implement AI-driven automation.
What’s best, automation systems don’t have to be overly sophisticated or expensive. Think about a simple conversational chatbot. Available via a mobile app, a website, or a self-service kiosk in the hospital hall, it assists patients 24/7 with basic contact information and directions or schedules an appointment and renews a prescription.
Another good example of an affordable, fairly simple AI-driven healthcare solution is robotic process automation (RPA). This involves bots that perform repetitive tasks, such as administrative data entry, document digitization, or processing billing and basic claims. RPAs immediately increase the speed of operations, free up personnel, and reduce human errors without the need for a massive investment.
“We must do a better job with our electronic health records. It takes up way too much time and it is taking clinicians and nurses away from their patients to the point where it is taking their joy away.”
Bernadette Melnyk, Ph.D., RN, APRN-CNP, is chief wellness officer of The Ohio State University and dean of the university's College of Nursing
[Source]
Lowering healthcare expenditures
Staff burnout and exhaustion is not the only issue that modern automation, data, and intelligence solutions help resolve. Integrating AI and big data into healthcare systems also drives sizable cost efficiencies. Administratively-oriented intelligence and automation software (which can be deployed on various portable and non-portable medical devices) keeps health providers’ precious dollars in their pocket primarily by alleviating the burden on clinicians and improving admin productivity. But there are more advantages.
Administrative waste generates billions of losses in healthcare every year, which can be recovered by AI-driven solutions in many ways. McKinsey calculated that by simplifying administrative spending and deploying intelligent technologies, healthcare organizations in the USA could save $265 billion annually.
Equipping patients with self-service software and devices (like mobile apps and self-service kiosks) and extending the functionalities of AI-driven patient portals and EMR systems translates to a lower load of administrative duties, shorter wait times, and eliminates unnecessary patient visits. In addition, modernizing the payment and billing system with targeted AI and deep learning models can simplify payments, streamline the revenue cycle management process, and assist with medical billing and coding.
Discovering new drugs
The process of discovering new drugs is extremely complex and involves a close examination of thousands of molecules to find the ones that might be potentially suitable for the drug. Consequently, the mean cost of discovering a drug is estimated at a jaw-dropping $747 million for dermatology drugs and up to $2.72 billion in the case of oncology and immunology therapies. In terms of time, drug research is not a walk in the park either—on average, it takes between six to seven years for a medicine to become available commercially!
Fortunately, AI models can make the hunt for new drugs quicker by rapidly processing vast data sets and making reliable predictions about their properties, adverse effects, and efficacy. As a result, enhancing laboratory and research devices with appropriate analytics and predictive algorithms may help drug companies save their constantly diminishing ROI.
This is just one of many applications of AI and analytics in the pharmaceutical context. The technology could also help improve medication adherence—a persistent issue that impacts treatment outcomes and recovery. For example, China introduced an AI-enabled drug intake tracking system in 2019. It merges data from pharmacy claims, lab and medical readings from medical devices, and other information to check whether patients comply with their prescribed treatment. AI and data analytics combined can also be useful in detecting medication errors or generating alerts when incorrect or missing components appear in a drug composition.
Managing chronic diseases
AI-driven solutions such as remote patient monitoring tools use different devices and analytical models to enable and enhance virtual care. They capture and analyze health data collected from wearables, mobile apps, IoT trackers, and other sources, automatically send updates to doctors, and trigger notifications when the readings deviate from the norm. These capabilities of AI-enhanced MedTech solutions make them useful for chronic disease management, where patients need to monitor, track and report new symptoms regularly.
Solutions leveraging AI and data show potential in chronic condition management as they facilitate self-management of diseases for patients. Additionally, by collating data from various devices and apps, AI-driven solutions offer a holistic image of a person’s health, providing clinicians with a fuller context of the disease and suggesting improved treatment options.
Additional resources
There are hundreds of scenarios for optimized healthcare delivery enabled by machine intelligence and data analytics solutions. We’ve only covered a few that we believe are the most likely to be prioritized in the near future.
If you’d like to learn more about the impact of data and machine intelligence on healthcare, we recommend some additional reading. It will allow you to replenish your knowledge and understanding of AI, ML, and big data applications in healthcare and MedTech.
- The FDA’s list of AI and machine learning-enabled medical devices marketed in the USA: Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices
- A comprehensive list of statistics presenting the landscape of AI and ML use: 100 Artificial Intelligence Statistics
- Insights on the impact of machine learning on healthcare: How machine learning is changing medicine and healthcare?
- IBM’s overview of AI medicine where you’ll find some more areas of AI application in healthcare: What is artificial intelligence in medicine?
- A detailed guide explaining how to implement artificial intelligence in any business: AI Business Guide
Mixed reality (AR & VR)
Mixed reality is another breakthrough technology that offers many exciting healthcare applications. Perhaps image-guided surgery is the first thing that comes to most people’s minds when they hear about virtual and augmented reality in healthcare, but the technologies’ use is much broader.
Apart from giving surgeons real-time information about a patient’s health during an operation, AR & VR solutions also help physicians gain a multi-dimensional view of health scans to understand the patient’s condition better. Mixed reality technology can also provide an extremely efficient medical training tool for aspiring surgeons to get a realistic perception of surgical procedures. Immersive learning using AR and VR headsets has also proven successful in training future nurses to respond to situations they are likely to encounter in their daily work.
More recently, the combination of real and virtual worlds has been found effective in physiotherapy. Integrated into motor training, mixed reality solutions allow patients to interact with a simulated multisensory environment in safe conditions. VR-based games and tasks are suitable for rehabilitation patients with varying degrees of motor deficits, from the injured to stroke victims.
Another fascinating field of virtual and augmented reality application in healthcare is psychotherapy. Delivering psychological therapies in mixed reality helps specialists treat anxiety disorders, phobias, addictions, PTSD, or eating disorders. For example, virtual reality exposure therapy helps patients fight debilitating fear or panic attacks by exposing them to triggers in a safe and controlled environment.
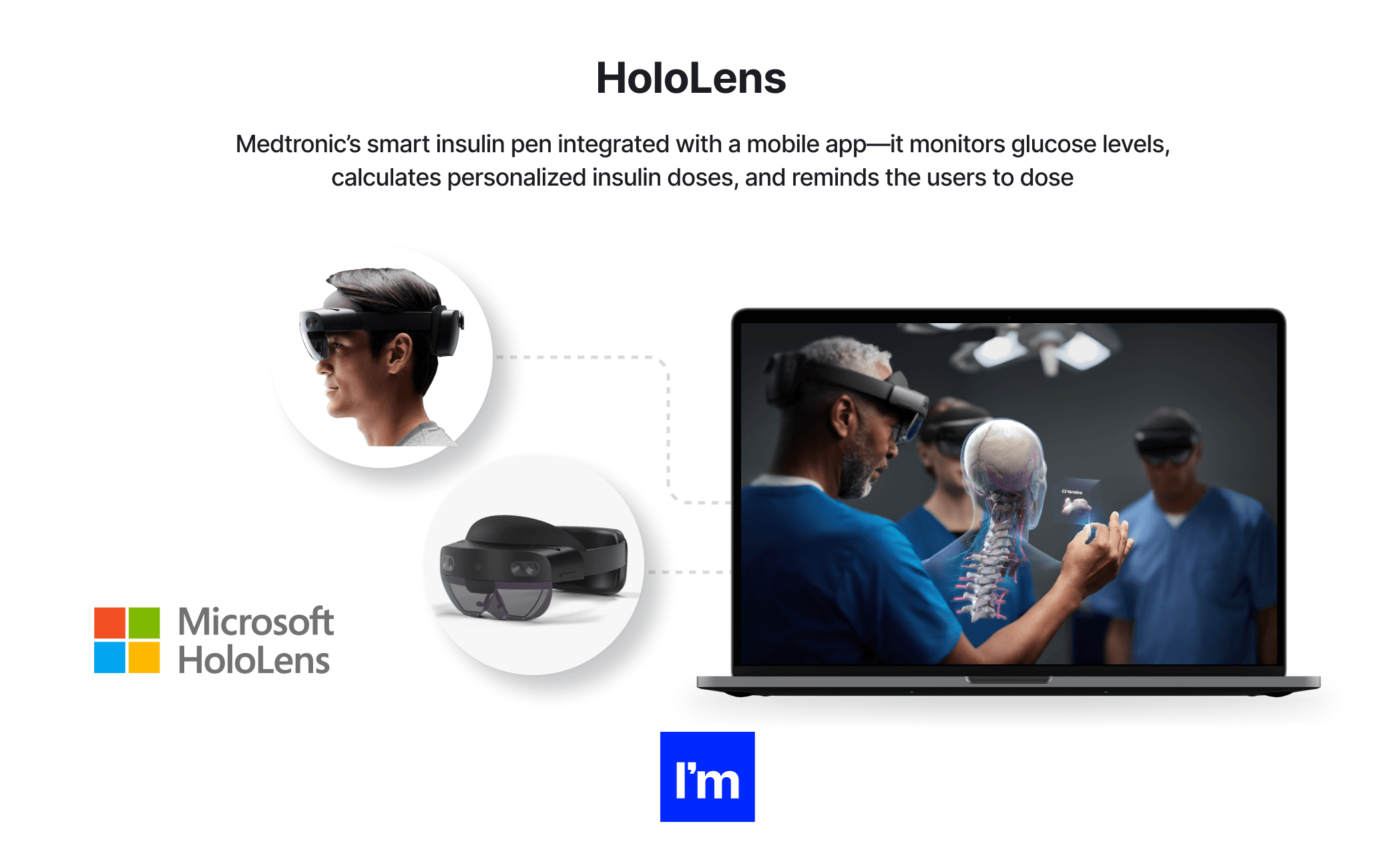
The immersive technologies also found a new use amid the pandemic. As an example, the HoloLens 2 headset by Microsoft enabled mixed reality medical ward rounds as a means to reduce the exposure of senior clinicians to patients infected with COVID.
Virtual reality vs. augmented reality
Often confused, virtual and augmented realities are separate, though related concepts.
As the name suggests, augmented reality adds to our real-world vision. It integrates digital elements into the surrounding environment, adding an overlay to the real image. Think Pokemon Go or Google 3D animals.
Virtual reality goes a step further, replacing the real-world setting with an alternative, virtual one. In addition, VR involves specialist gear, such as a headset, to produce the virtual image, while AR usually only requires a smartphone, computer, or another piece of equipment.
Elements of VR and AR, when combined, constitute a mixed reality.
Business potential
The global mixed reality healthcare market size is expected to reach $1.33 billion by 2027, growing at an astounding CAGR of 47.2 percent over the forecast period. One of the main factors contributing to that success is the technology’s versatility. The technology can be deployed at all stages of the healthcare cycle, including training and prevention.
Mixed reality solutions are extremely helpful, and not just for surgeons. Psychologists, physiotherapists, family doctors, and speech pathologists, among others, can also integrate mixed reality experiences into their fields to enable personalized treatment plans, enhance the patient experience, and drive more informed and accurate diagnoses. Moreover, VR and AR are still in their infancy, which explains their explosive growth rate and provides opportunities for a lucrative investment.
Barriers to adoption
VR and AR technology creates new possibilities to provide highly personalized care, especially for underserved patients. Yet despite its unique capabilities and vast business potential, it still has to tackle several barriers before it permeates the mainstream.
First of all, healthcare providers in many countries still struggle with the lack of reimbursement for mixed reality-based treatment plans. Secondly, the low level of familiarity with mixed reality tools makes healthcare providers resistant to their use. Finally, technical limitations, such as limited availability and access to the underlying infrastructure or incompatibility with other healthcare platforms, also stymie broader adoption.
Even with these challenges, the growing exposure to consumer AR and VR solutions shines the beacon of hope for the technology’s use in healthcare, especially as companies like Microsoft, Google, and Facebook/Meta increase their investments in its adoption, including in the context of medical care.
Underlying software
The type of software for virtual and augmented (and mixed) reality solutions varies across their types and applications. Since AR can be used with mainstream smartphones and tablets, it requires different software than VR, which is based on dedicated hardware.
Depending on the device, the software needed to create virtual worlds will provide data storage and management, image recognition and manipulation, movement tracking, sound recognition, voice navigation, 3D graphics, and motion graphics.
To develop applications for a specific piece of hardware, MedTech engineers use software development kits comprising libraries, samples, guides, tutorials, and blueprints that help them code faster. Game development additionally requires a game engine that integrates with designer tools and CAD software to create realistic, immersive experiences.
Examples of existing solutions
- Surgical Theater - A “surgical rehearsal platform” for neurosurgical procedures. Surgical Theater
- Microsoft HoloLens - A mixed-reality holographic device that can display information, blend virtual elements onto a realistic display, or simulate a virtual world. HoloLens
- XR.Health - A virtual treatment room enabling engaging, game-like therapy. XR Health
Mobile and telehealth solutions
In a world where 7.9 billion people use 15 billion mobile phones, it is only natural for the healthcare industry to tap the potential of mobile devices for making healthcare more accessible, personalized, and affordable.
What is mHealth?
mHealth, or mobile health, enables fast and convenient access to healthcare services, from disease prevention to primary and follow-up care. Many mobile apps support both patients and doctors in delivering targeted, optimized care. We will find solutions that support clinical diagnosis and decision-making, encourage patient engagement and behavior change, help improve drug adherence and treatment compliance or deliver healthcare education.
What is telehealth?
Mobile health belongs to a wider group of telehealth solutions. They incorporate all instances of remote healthcare delivery via digital technologies, not limited to mobile devices. Additionally, while mHealth is usually solely focused on patient-to-provider interaction and helping people look after their health, telemedicine solutions encompass a variety of interactions between patients and clinicians and among clinicians themselves. Examples of telehealth solutions include live video conferencing, remote patient monitoring tools, remote collaboration tools for clinicians, and virtual care stations.
What is eHealth?
eHealth refers to the practices of supporting and delivering healthcare via electronic means. It encompasses electronic health records, lab systems, patient portals, and similar solutions. While the term is sometimes confused or used interchangeably with telehealth, it does not necessarily need to include software and devices that enable remote care (like telehealth). Additionally, telehealth is usually used more specifically in the context of patient care. In contrast, medical and non-medical staff can also use eHealth for activities and transactions unrelated to the patient.
Among the many benefits that telehealth and mHealth apps bring to the table, several deserve particular attention. First, strengthening healthcare delivery with mobile applications makes patients more self-reliant and empowered to make decisions about their health and well-being. For example, one study by PwC found that 44 percent of patients use mobile apps to monitor their wellness. Almost the same number (43 percent) use digital devices to connect with their provider.
Another important benefit of remote and mobile healthcare delivery is that they may positively affect overall patient outcomes by informing the users about upcoming doctor’s appointments or reminding them to take medicine. Moreover, health data collected by mobile applications and software integrated with biosensors and trackers are far more reliable than self-reported patient symptoms. Health providers can also manage them more consistently.
In addition to these advantages, all solutions that enable remote patient monitoring, communication, and treatment democratize access to healthcare and increase doctors’ and patients’ safety. For example, in the study mentioned above, 59 percent of patients said that obtaining advice via mHealth solutions had replaced some visits to doctors.
This knowledge is essential in social distancing and disease spread prevention measures, but there’s also another gain in broadening healthcare access. Namely, as the COVID-19 pandemic has put health inequities on full display, telemedicine, including mobile health apps, gives providers a chance to build a more equitable system.
Business potential
If we consider the above benefits and the role of telehealth solutions (including mHealth apps) in patient empowerment, we can safely assume they will become permanently integrated into established treatment practices. The global telehealth market is already worth over $40.3 billion. By 20230, researchers expect it to increase by nearly six times.
The main factors facilitating this growth include the increasing availability of mobile and digital technologies, the expanding network connectivity, robust competition driving greater innovation and lower pricing, growing digital literacy, and the increasing support for digital health platforms and apps from medical professionals and governments alike.
When discussing the drivers for adopting telehealth and mHealth solutions, we cannot ignore the immense impact of COVID-19. The global crisis catalyzed the development of solutions enabling remote consultations and safe healthcare delivery.
Barriers to adoption
Technological and infrastructure barriers remain key inhibitors to expanding telehealth solutions in some countries. The adoption of digital platforms enabling remote consultations and monitoring involves installing expensive equipment and deploying high-bandwidth networks, especially on the healthcare providers’ side.
Additionally, even though the legal framework for adopting digital solutions in healthcare is continually evolving in many places, it often remains unclear how the use of data in digital and mobile apps is regulated.
Underlying software
When speaking about mHealth solutions, we usually refer to mobile apps installed directly on mobile devices such as smartphones or smartwatches that deliver a particular functionality. They should be available on different systems and devices to reach the broadest possible patient population.
Telemedicine software usually runs on computers or servers, but it can also be available in the cloud as a SaaS (Software as a Service) platform. Telehealth platforms comprise functionalities such as video chat, patient documentation management, online prescriptions, billing, and integrations with other essential programs and systems. These solutions must remain compliant with the existing health and data protection regulations (e.g., HIPAA for the USA or GDPR for the EU).
Examples of existing solutions
- MyChart - A mobile app that allows users to access medical reports, test results, medication, prescriptions, bills, and other data. MyChart
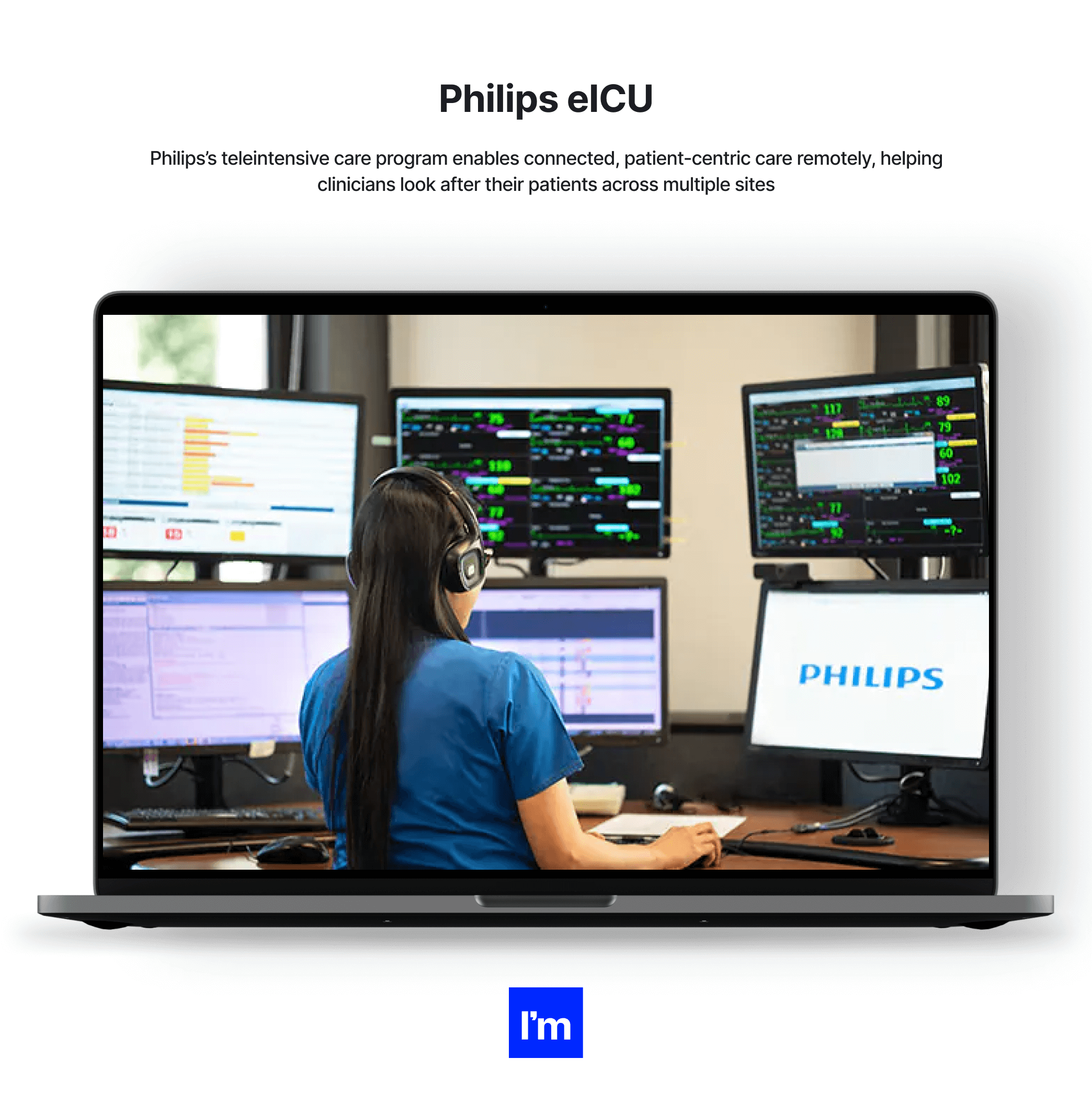
- Philips eICU - A centralized remote care solution for monitoring intensive care unit beds. Philips eICU
- Welldoing - A British telehealth service providing access to virtual therapists. Welldoing
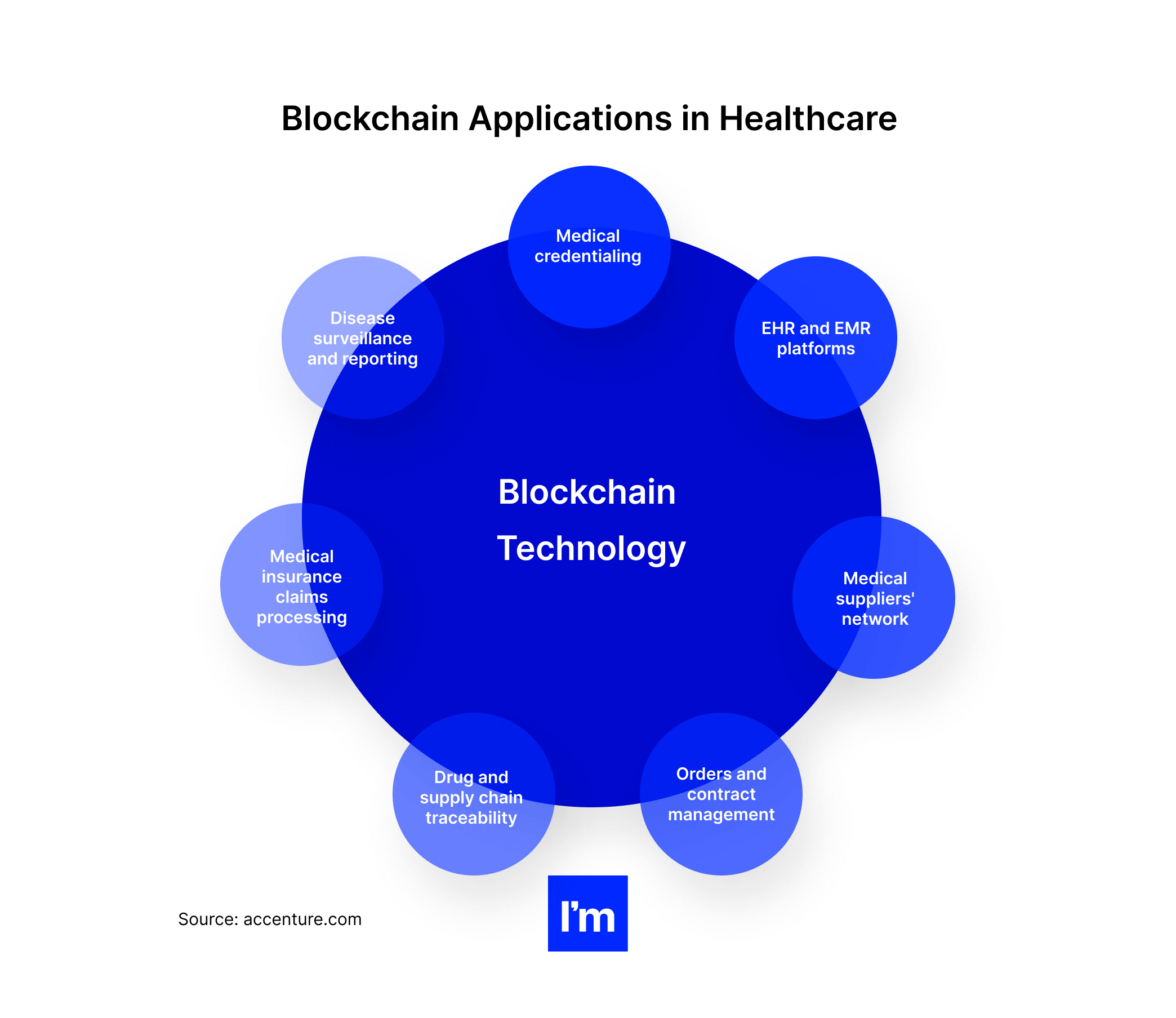
Blockchain applications in healthcare
When discussing MedTech, we cannot ignore blockchain technology. The inherent benefits of this shared, distributed system, such as immutability, security, consistency, and verifiable identity of all transaction participants, make it highly relevant in the healthcare industry.
Blockchain technology has a wide range of applications in healthcare, especially as organizations adapt their supply chains to ensure expedient preventive solutions and extend services online.
Blockchain technology helps healthcare providers ensure data integrity and security by enabling trust, transparency, and collaboration. It also helps reduce potential errors and fraud in drug production and supply or counterfeit prescriptions, doctor’s certificates, and insurance claims.
The technology performs particularly well in all areas that require scrupulous and transparent recording and tracking information. It can also ease data transfers between multiple actors while providing reliable verification and authentication. Therefore, blockchain technology is highly suitable for solutions enabling real-time payments and settlements as a technology well-embedded in financial operations.
Here are some specific use cases for healthcare that blockchain technology can help deliver:
- Verification of health credentials. Blockchain technology can be groundbreaking for medical credentialing as a technology that hands over the control over data to the providers, who can choose with whom and when to share it. In addition, as a decentralized, scalable solution, it helps ensure data transparency and traceability. One example is the ProCredEx blockchain platform, which allows credentialing organizations to share, exchange, and monetize verification data.
- Management of electronic medical records. As a decentralized platform, a blockchain allows equal access to medical services for all involved healthcare providers and the patient. Furthermore, advanced cryptography ensures all transactions are secured and cannot be tampered with or deleted. Besides, every authorized party gets updates on data changes in real-time. These features make blockchain technology ideal to underpin modern EHR and EMR platforms.
- Sourcing and onboarding medical suppliers. Healthcare companies may also leverage blockchain technology to address equipment shortages and accelerate supplier onboarding. For example, in 2020, IBM launched a blockchain network to identify and onboard vendors to facilitate access to a broader range of suppliers for government agencies and healthcare organizations. The idea was born in response to the healthcare crisis and supply chain shortages brought by the COVID-19 pandemic.
- Managing service contracts and orders. One of the primary uses of blockchain technology is automatically executing a smart contract once all predetermined conditions are met. Doing so removes the admin burden, streamlines complex processes, and ensures the security and confidentiality of data and the involved parties. These blockchain functionalities find use in healthcare contract management software and apps.
- Tracing and securing drugs and medical supplies. The medical supply chain is another interesting area for blockchain use. Interoperable blockchain systems, such as this one devised by a group of Swiss hospitals, can transform how medication and supplies reach patients and providers. They are tamper-proof, auditable, and timestamped. In addition, they enable efficient tracking and tracing of events in the supply chain, providing detailed information about each transaction, participant, location, time, and other crucial factors.
- Processing insurance claims. Implementing blockchain technologies can be very beneficial, as they can help verify medical bill information, handle patient claims, and automate the whole process, together with payments. Blockchain-based medical insurance claims processing primarily allows patients to submit claims quickly while also providing an efficient tool for combating fraud.
- Disease reporting and tracking. The pandemic has revealed another practical use of blockchain technology for disease surveillance and case tracking. As usual, distributed ledger platforms offer unmatched transparency, traceability, and immutability of data and transactions. In addition, blockchain-based surveillance systems come with the extra benefits of scalability, embedded security, and excellent interoperability, making real-time disease tracking more efficient and accurate.
Digital disease surveillance
Digital health tracking tools are another mature innovation in MedTech that gained traction in the wake of COVID-19. The technology refers to the systematic collection and interpretation of digital data collected from social media and other internet sources to track and manage the spread of infectious diseases.
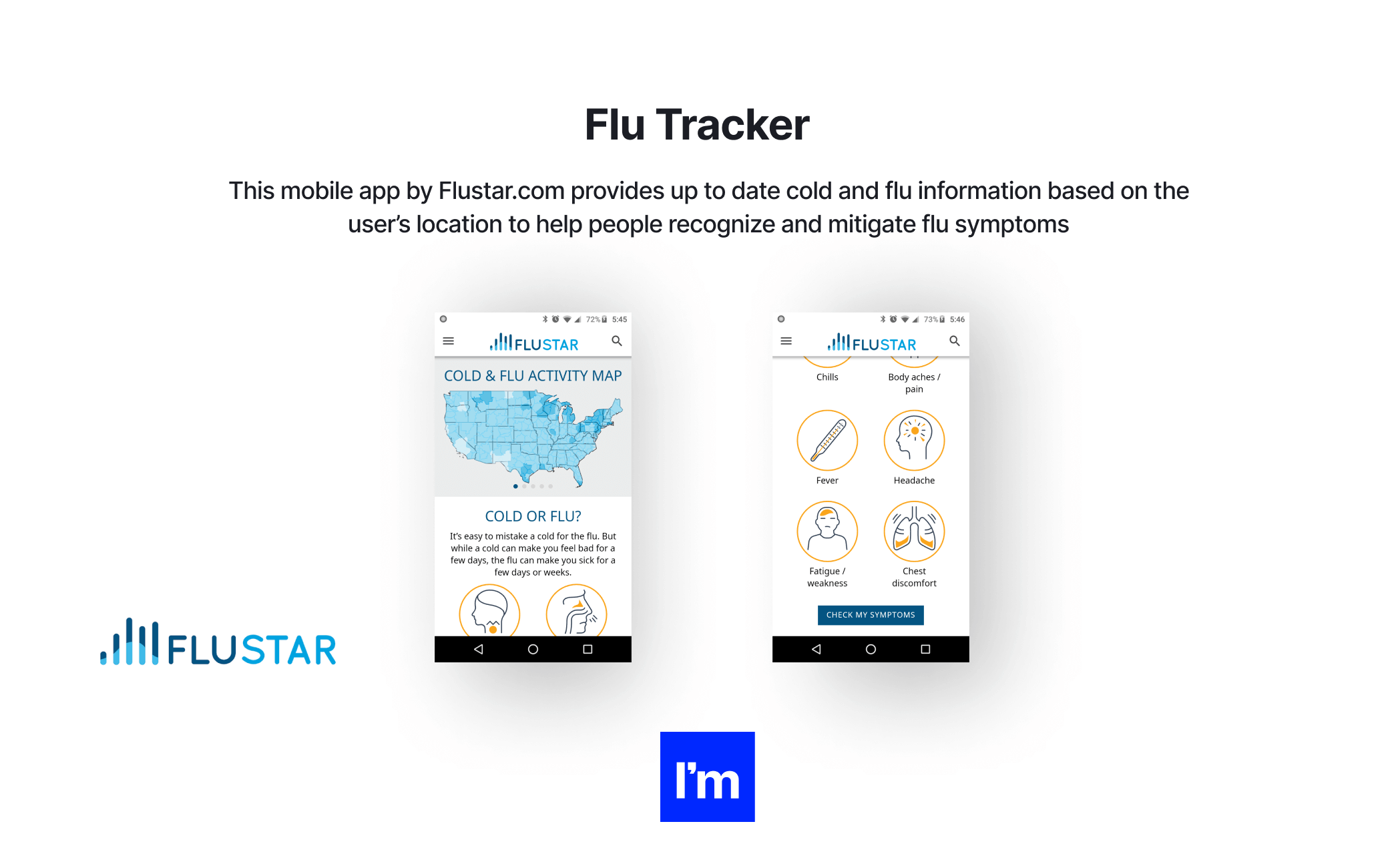
Digital surveillance systems vary from moderated web databases to real-time mobile apps, but they share common goals and work similarly. The data collected by these systems, whatever it might be—information about an infection submitted by the user or web searches for flu symptoms—are primarily used to track the incidence of diseases in real-time and forecast possible spread patterns and risks.
In the past, countries used digital disease surveillance systems to detect swine flu early and manage the spread of the Ebola virus. As a result, flu tracking solutions have become ubiquitous, both as websites and mobile apps. Several tools have emerged focusing specifically on monitoring the spread of COVID-19 instances (e.g., a crowdsourced site Outbreaks Near Me).
“We are on the precipice of an unprecedented opportunity to track, predict and prevent global disease burdens in the population using digital data.”
Allison Aiello, The Gillings School of Global Public Health
Business potential
The recent pandemic has underscored the importance of monitoring and forecasting the risk of disease spread in real-time. Based on the analysis of data submitted digitally by populations, researchers can also determine which individuals are more likely to develop severe symptoms and require hospitalization with high accuracy.
The immense potential of digital surveillance tools consists primarily of how they allow health officials to spot outbreaks. Additionally, the predictions based on the information aggregated from various sources (including social media, public health data, crowd-sourced data, web searches, and more) are highly accurate, partly due to the huge volume of collected data.
Main drivers for the continued adoption of digital disease surveillance apps include:
- A steady increase in global internet usage
- Mainstream use of social media (82 percent of people in the US have at least one social media account)
- The growing use of mobile phones, including in low and middle-income countries
- Ease of use of the tools and high perceived benefit for the users
Barriers to adoption
As it’s in the case with IoT devices, concerns related to the users’ privacy may be the main barrier to adopting data-based solutions in healthcare. Considering the sensitive nature of health data, the risk of privacy abuses is significant, which may deter potential users.
On the other hand, many countries have already introduced laws to protect privacy on social media and the internet in general. Additionally, measures such as data anonymization, encryption, and enforcement of informed consent help safeguard the identity and privacy of the users.
Underlying software
Digital disease surveillance systems usually comprise a database that connects to the selected data sources and supports data sharing, integration, and coordination. In addition, they should provide the scalability required to account for the growing data volumes and be easily configurable to changing protocols and geographic locations. Finally, these platforms should be intuitive to enable quick data entry and sharing on the user's end.
Examples of existing solutions
- SORMAS - A real-time open-source electronic tool for disease surveillance and outbreak response. SORMAS
- VAERS - An open database and online search tool containing vaccine adverse events reports. VAERS
- Flu Tracker - One of several mobile apps providing up-to-date cold and flu activity information based on the user’s location. Flu Tracker
Digital health software solutions
Driven by the growing emphasis on proactive and personalized patient care, digitalization in healthcare is in a state of continuous development. Moreover, the exponential growth in health data calls for more software in medicine.
While the industry has been notoriously reluctant to adopt IT technologies, healthcare professionals changed their attitude between constant lockdowns and the shift to telemedicine imposed by the pandemic. As in-person non-urgent care services ground to a halt at the pandemic’s peak, many of them moved online, hoping to build resilience in tough times and maintain the level of service.
And indeed, these tactics proved successful, as 51 percent of patients surveyed by Accenture said they hadn’t noticed any change in the access to healthcare services since the onset of the COVID-19 crisis, while 26 percent more pointed out that it had even improved.
And what kind of software do healthcare organizations use to enhance the delivery of patient care and make their staff more productive? Let’s briefly review the most popular of them.
EHR/EMR software
Electronic medical documentation (EMR—electronic medical records and EHR—electronic health records) has become a standard solution in modern healthcare facilities. Indeed, according to the CDC’s data, nearly 90 percent of US office-based physicians use an EHR system.
Considering the scope of features these solutions offer, it's hardly surprising. Even so, many of these platforms leave a lot to be desired, especially if they are poorly integrated with other systems and apps, or based on legacy technologies and running locally, instead of in the cloud.
“We must do a better job with our electronic health records. It takes up way too much time and it is taking clinicians and nurses away from their patients to the point where it is taking their joy away.”
Bernadette Melnyk, Ph.D., RN, APRN-CNP, is chief wellness officer of Ohio State University and dean of the university's College of Nursing
[Source]
EMR and EHRplatforms collect and centralize all patient information and treatment history, provide data reporting and visualization, enable invoicing, payments, reimbursements settlements, and extend patient portals for self-service. They also streamline patient-provider communication and allow clinicians to stay on top of their patient's health data.
Examples: Epic EMR, GE Healthcare, Praxis EMR, CareCloud, Nextech

Healthcare staffing software
The healthcare industry is permanently understaffed. To that end, healthcare staffing systems can help find and recruit qualified personnel faster and more efficiently. These are all-embracing HR systems that streamline the entire recruitment lifecycle through automation and integration with other systems and services. As a result, staffing agencies and internal HR departments in clinics, hospitals, and other medical facilities use them to become more productive and shorten their hiring process.
Designed with compliance and audit trails in mind, healthcare staffing solutions improve placements for permanent and temporary positions, allowing organizations to fill vacant positions faster, onboard new hires more easily, and effortlessly manage staff, finances, and credentials.
Examples: Erecruit, NextCrew, AkkenCloud, 1Staff
Medical inventory software
Medical device management software helps visually track medical supplies and equipment in real-time and identify their details, like location, price, condition, quantity, etc. Hospitals use it to streamline facility logistics and automate manual stocktaking. In addition, these systems usually include an asset reservation and scheduling module, a certificate retrieval system, invoicing functions, and integration with third-party systems.
Examples: HospiLogix, Sortly, Hybrent, Medstar HIS, Arbimed
Hospital management software
These platforms are more comprehensive than inventory systems and facilitate day-to-day hospital operations for doctors, nurses, and admin staff. They streamline the management of all paperwork related to each patient, automate workflows, and simplify tasks.
HMS solutions help with patient admissions and discharge, updating lists of doctors and nurses, keeping track of appointment dates, managing HR and payroll, tracking bill payments, issuing invoices, and more.
Examples: Medstar HIS, Docpulse, SoftClinic, RicohDocs
Medical imaging software
As the name suggests, this type of software helps medical professionals create, track, store, manipulate, and manage patient images. It uses deep learning algorithms to quickly read and analyze images and identify anomalies.
Medical imaging systems primarily process CT, MRI, PET, x-ray, and other scans. However, some solutions also allow technicians to create 3D models of medical equipment or human body parts.
Examples: Arterys, UltraLinq, Carestream RIS, Merge Healthcare
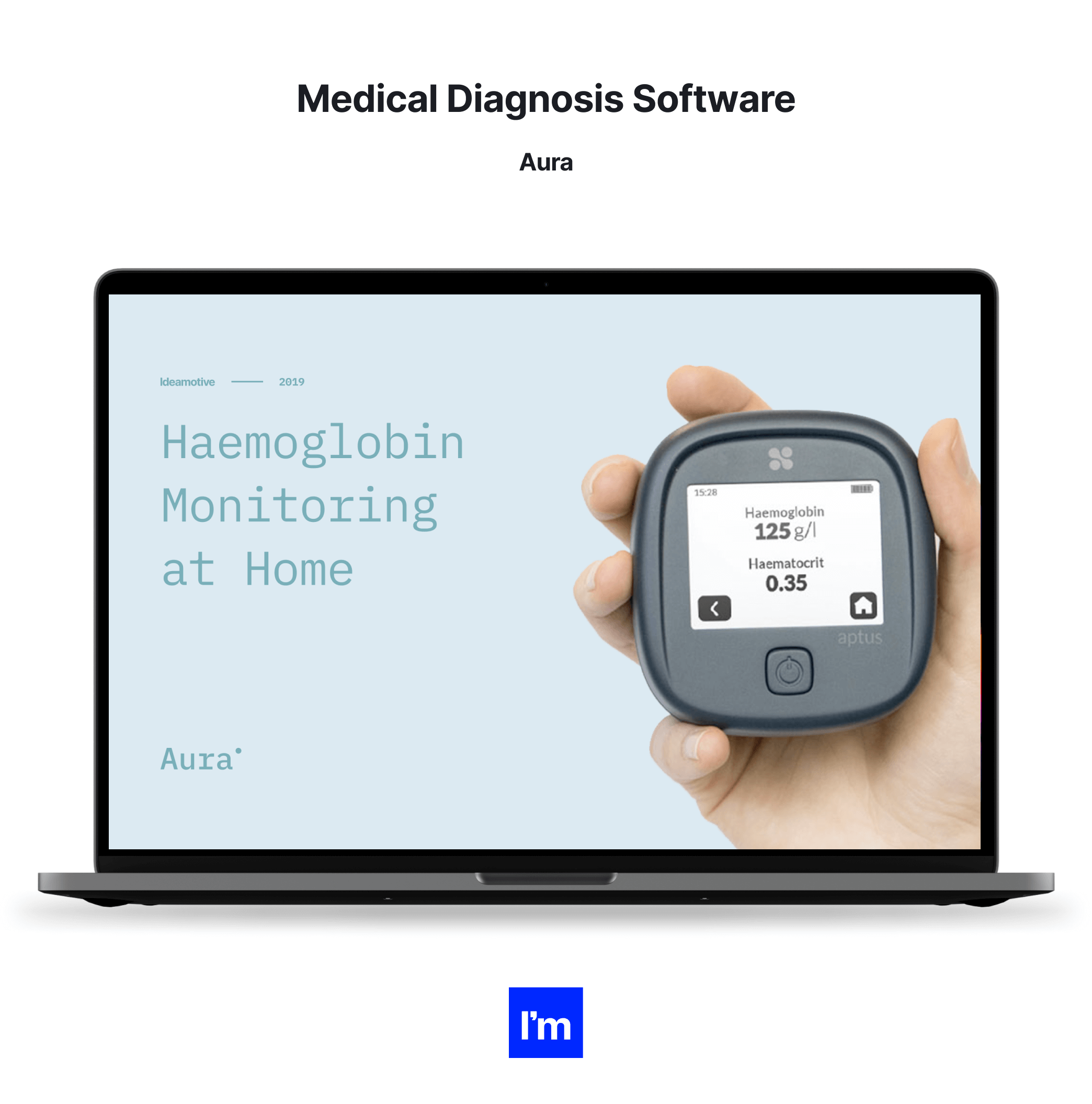
Medical diagnosis software
AI-powered medical diagnosis solutions ensure accuracy and minimize the risk of error in diagnosis. They handle information from medical equipment and other sources to produce reliable results.
Medical diagnosis systems typically support clinicians in making a correct and quick diagnosis, reducing manual processes, and identifying specific patterns. However, apps such as symptom checkers and self-diagnosis tools also allow patients to determine if they should seek a doctor’s help.
Examples: folio3, Symptomate, YourMD, FPT Software, Zühlke
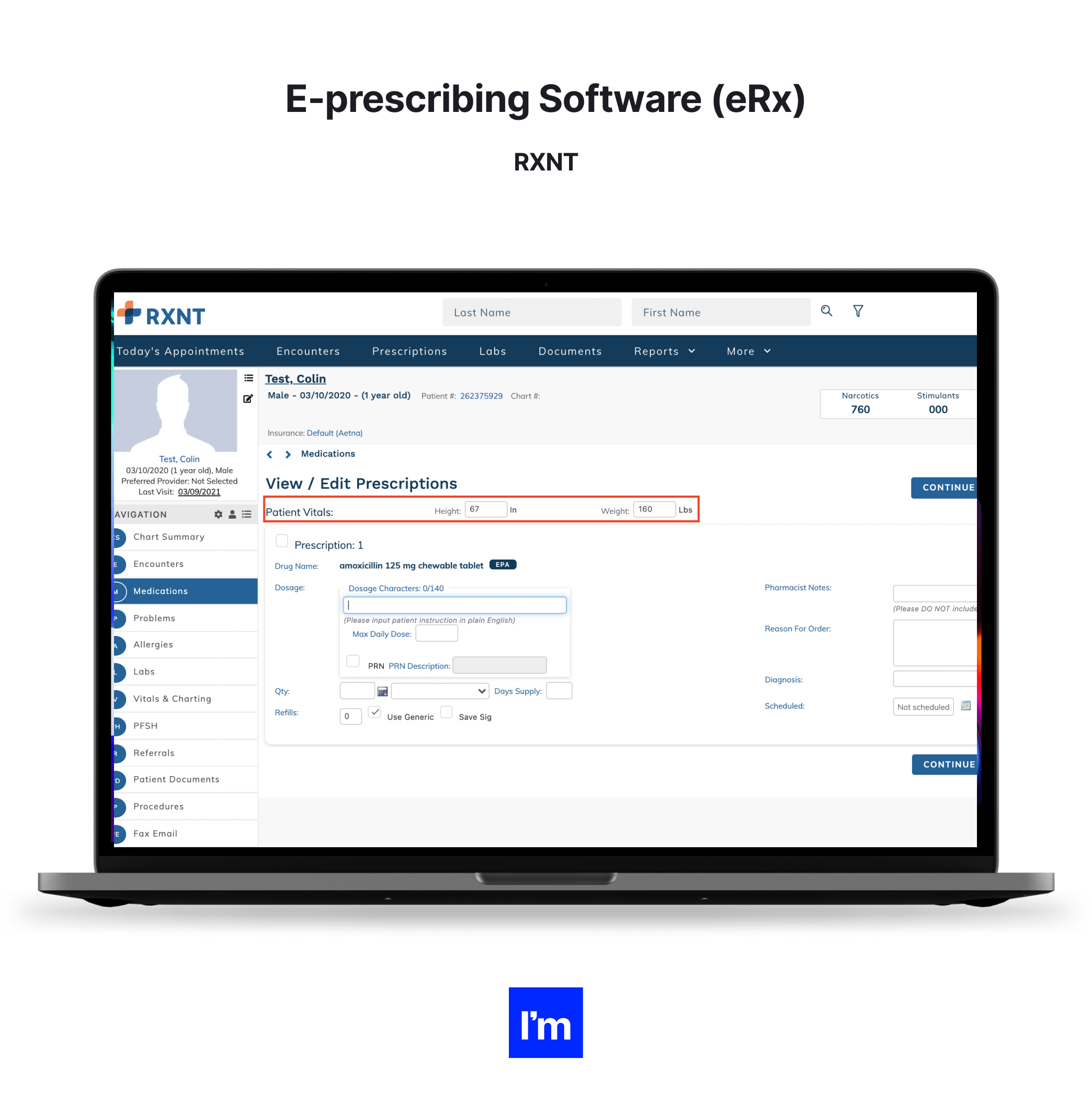
E-prescribing software (eRx)
Electronic prescribing software helps physicians and practice administrators save time with an efficient digital process. It allows healthcare professionals to easily browse and select drugs in a database, check drug and dosage information, and create and electronically send a prescription to the patient without the need for an on-site visit.
The top solutions are fully compliant with the healthcare and data protection regulations, offer secure data handling capabilities, and often come with e-prescribing mobile apps.
Examples: MDToolbox, RXNT, MediTab, ScriptSure
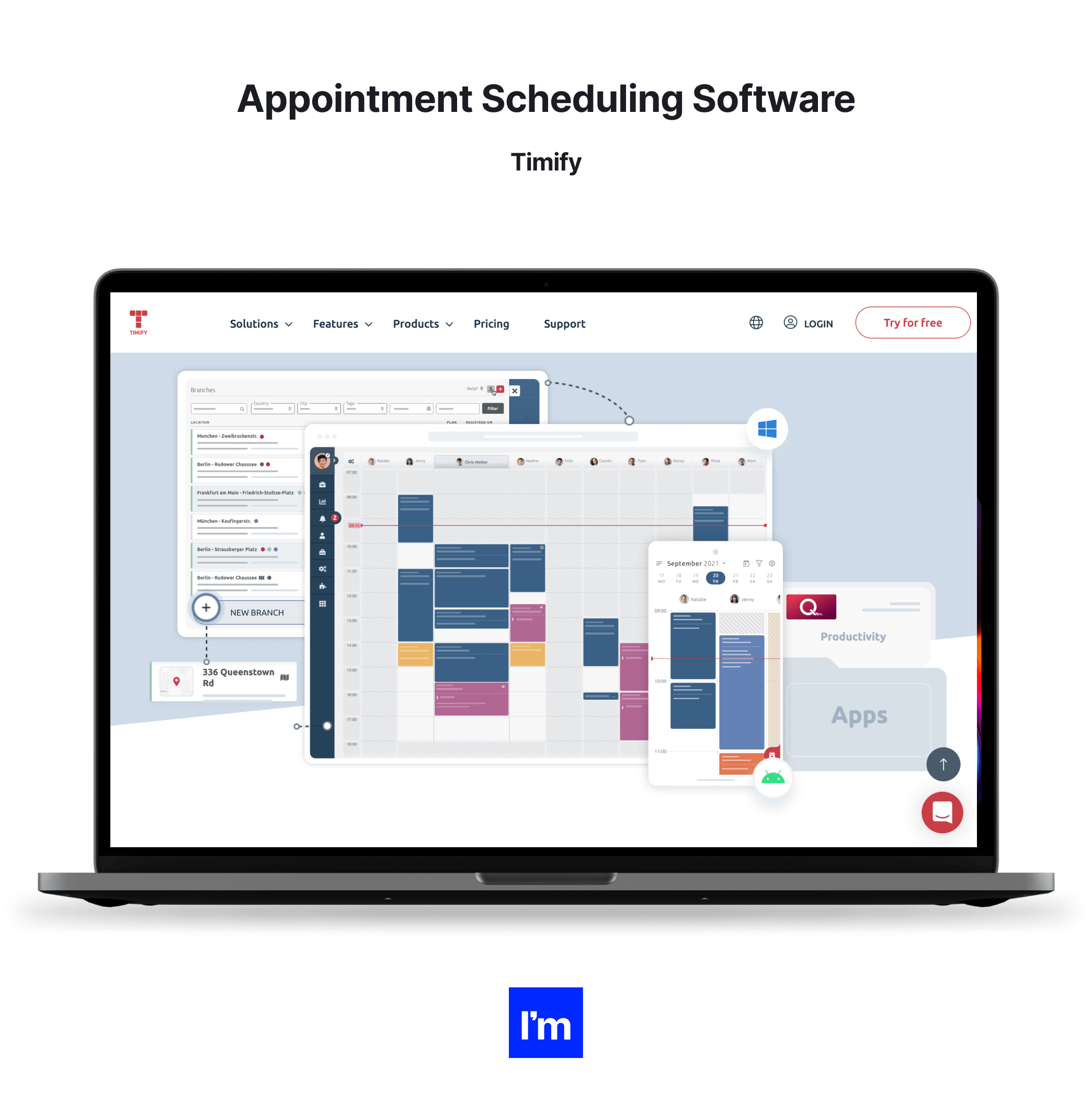
Appointment scheduling software
Healthcare scheduling software automates the patient booking process for medical offices. It coordinates the clinicians’ calendars with patients’ requests for visits, confirms available time slots, and sends out appointment reminders.
Other features found in advanced healthcare scheduling software include dictation-based appointment booking, real-time location tracking, an offline mode, and suggestions on the best route to reach the facility.
Examples: Timify, Skedulo, SimplyBook.Me,
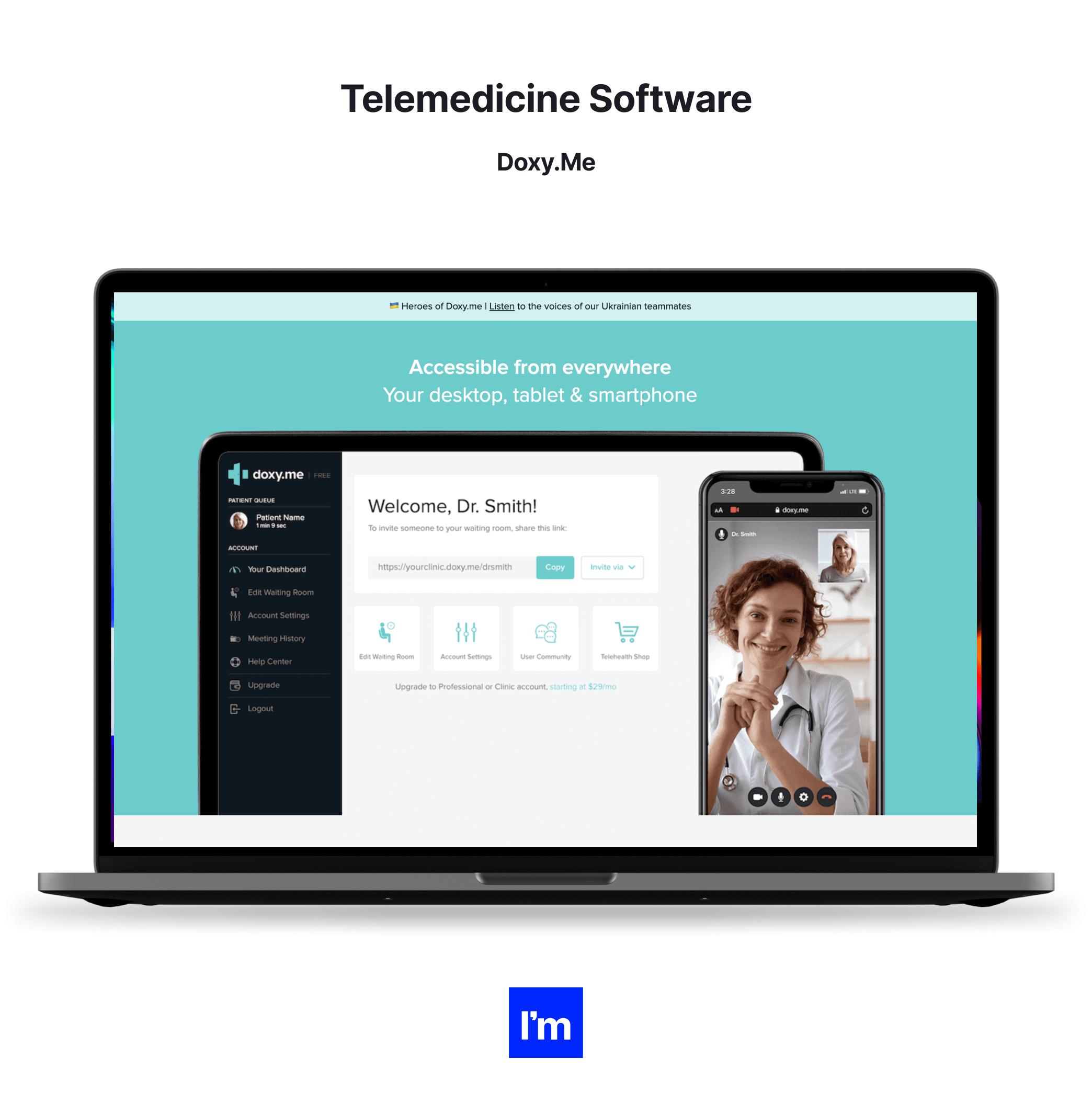
Telemedicine software
We couldn’t forget telemedicine platforms that enable remote patient visits. These solutions combine video conferencing, instant message chat, and voice calls with image sharing and clinical documentation to meet patient needs for virtual care delivery.
Some telemedicine platforms additionally feature billing modules, virtual waiting rooms, and e-prescribing features. However, regardless of the functions offered and the device used for e-consultations, all telemedicine systems must include data encryption and security features to ensure data safety and confidentiality.
Examples: SOC Telemed, Doxy.Me, Chiron Health, Avizia, MD Live
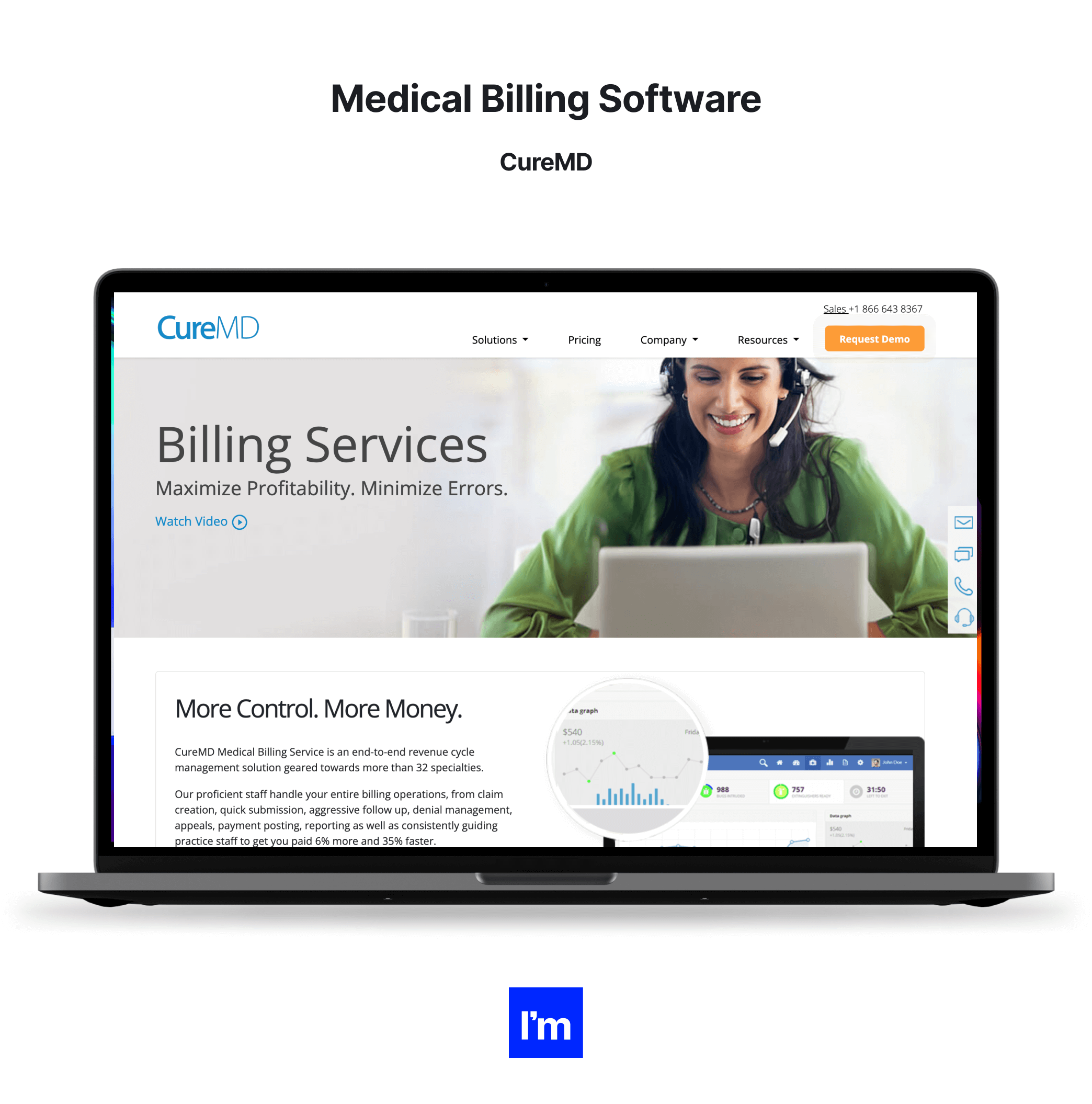
Medical billing software
Medical billing applications automate the healthcare billing process. They help practices and hospitals process invoices, payments, insurance claims, and other issues related to finances. Advanced billing software offers extensive analytics and reporting functions and can even include predictive components to optimize financial decision-making for healthcare facilities.
Apart from systems used specifically for billing and payments, many companies also use healthcare contract management software for settlements with third parties and subcontractors.
Examples: NextGen, AdvancedMD, EpicCare, CureMD, DrChrono
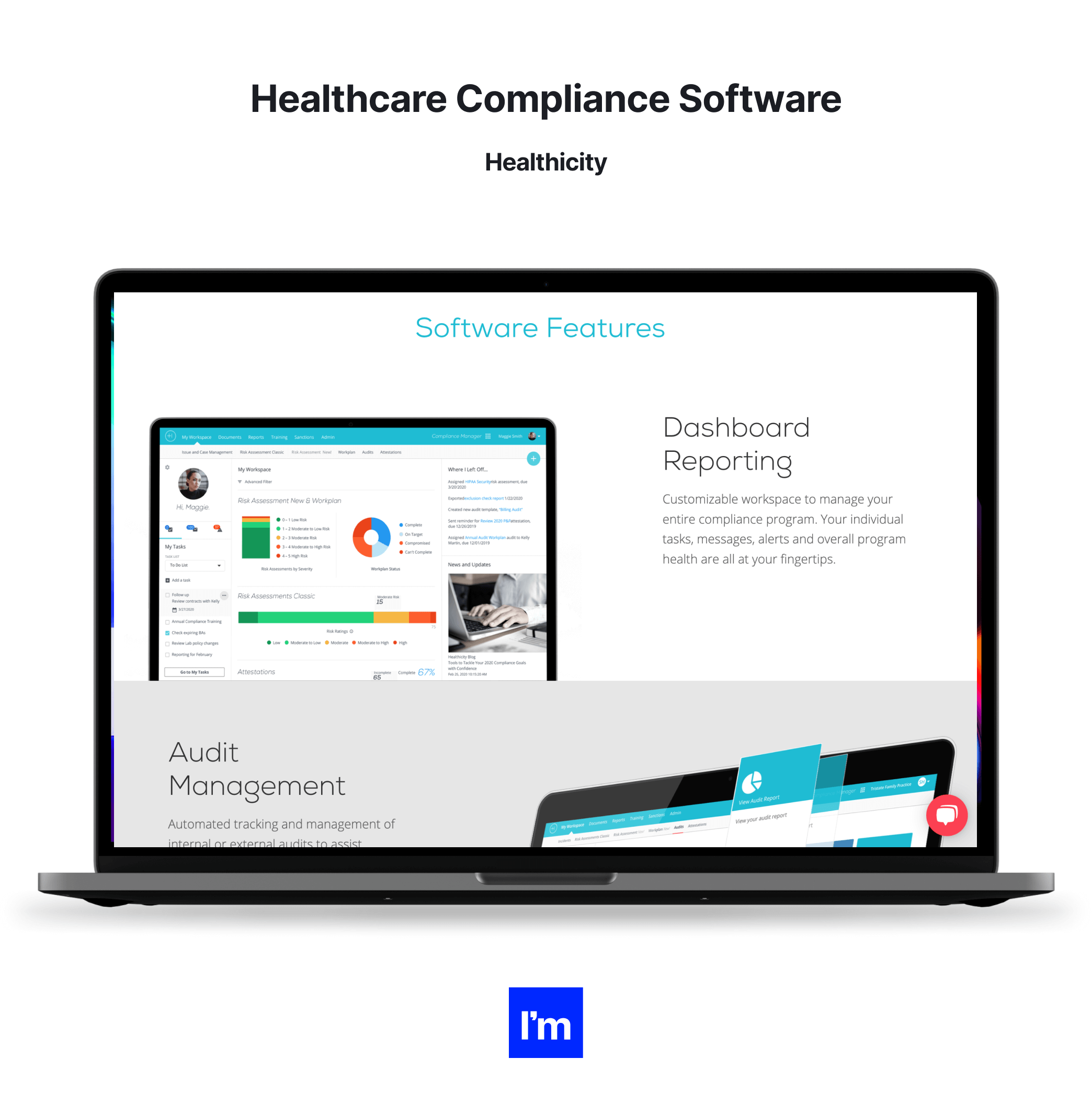
Healthcare compliance software
This type of software ensures that healthcare organizations adhere to compliance guidelines and regulations. It supports incident monitoring, reporting, auditing, conducting risk assessment, and training personnel.
Healthcare compliance platforms include automated audit tracking and management, customizable dashboards with alerts and visualization, and incident management modules. Altogether, they facilitate the deployment and maintenance of audit and regulatory compliance.
Examples: Healthicity, MedTrainer, HIPAAReady, Dude Solutions
03 MedTech and digital medicine benefits, challenges, opportunities, and risks
We hope you can now see that the introduction of MedTech into modern healthcare systems is not a question of ‘if,’ but ‘when’ and ‘how.’ But before we dive into the development of medical technology solutions head-first, let’s consider several key aspects.
This section looks into the advantages and disadvantages of MedTech, opportunities for healthcare organizations, and risks and challenges that they may face when adopting medical technologies.
Key benefits of MedTech and digital health
The overarching aim of MedTech and digital health solutions is to enable the early and precise diagnosis of health issues, empower patients and clinicians to deal with them with minimal disruption and improve the treatment outcomes, health, and wellbeing of all populations. Breaking this goal down into specific benefits for all parties involved, we can identify the following advantages:
Cost-cutting
Even though the initial investment in digital healthcare may seem steep, the long-term impact of implementing MedTech pays off, even driving further cost savings. That’s because by enabling more effective, individualized treatment, emphasizing prevention and early detection, and empowering patients, digital medicine and MedTech solutions facilitate cost-effective care.
Medicine technology also speeds up recovery and helps reduce hospital admissions while streamlining practice and hospital workflows. All of that contributes to less expensive and more efficient treatment plans—leading to a more affordable system for all participants.
Higher efficiency
Innovative software and devices improve care coordination and automate tasks to unlock efficient healthcare delivery. For example, EHR systems, medical billing platforms, and other MedTech and digital health software help practices and hospitals run smoothly by facilitating communication and enabling faster data retrieval, transfer, and sharing.
Time savings
Time savings accompany greater operational efficiency. And healthcare software solutions enhanced with RPA and machine intelligence components can take over repetitive administrative tasks that usually devour a significant portion of each medical and non-medical employee’s life.
Whether you need to support office admins retrieving the patients’ data or unburden doctors spending too much time on paperwork, digital healthcare software and devices can do that. Increasing patient engagement, mobile healthcare apps, monitoring devices, and patient portals reduce the need for doctor visits, which also adds to time savings on the patient’s and clinician’s end.
Healthcare accessibility
Making healthcare more affordable and accessible is an important goal of medical technologies, particularly telehealth solutions. MedTech devices and apps inform patients of the state of their health and navigate them through the next steps without the need for a doctor’s appointment. They can monitor the user’s condition remotely, saving them time and money on visits and reducing their risk of exposure.
More informed decisions
Accurate and timely diagnoses thrive on data. The more insights into the patient’s health, symptoms, and lifestyle a doctor has, the more precisely they can determine the best treatment. And here’s where MedTech contributes immensely, producing, collecting, and analyzing a full amount of data that inform correct diagnosis and treatment plans. Solutions comprising big data analytics and AI algorithms deliver insights based on information about an individual patient, extrapolate population trends, and identify and mitigate care management gaps.
Improved outcomes
Sensors, wearables, mobile trackers, and other MedTech devices provide crucial healthcare information in real-time or nearly instantly. On top of that, results and readings from advanced lab and imaging technologies supplement this data. This knowledge helps doctors detect potential issues faster to assist patients with early interventions to reduce risks, choose targeted treatment, and help patients recover more quickly.
Better care coordination
Health issues don’t occur in isolation. By amassing, integrating, and sharing health information with all parties, MedTech and digital medicine facilitate holistic care delivery, offering a broader view into each patient’s physical, mental, and social needs. Solutions like EMR and EHR systems collate data gathered from tests, examinations, wearable devices, etc., making them accessible to patients and clinicians in different specialties.
Reduced human errors
Data entry errors, vague or exaggerated self-reported symptoms, non-adherence, and other human factors negatively impact treatment efficiency. MedTech deals with that issue in numerous ways. For example, bar-coded medication administration and electronic drug reconciliation, in combination with drug tracing devices and apps, help prevent medication errors. Modern electronic health record software uses templates, disease code error detection, speech recognition, and patient portal integration to cut down on typing errors. Meanwhile, wearables and remote trackers provide accurate readings that can supplement the patient’s self-reported medical history for a full picture of their health.
The value of medical technology: Who benefits?
The most obvious answer is ‘patients.’ Of course, patients are the cornerstone of all medical progress, with innovations in MedTech that focus on enhancing patient well-being and improving treatment outcomes. However, MedTech delivers value to various beneficiaries through innovative devices and diagnostics. Check out how the MedTech industry supports different individuals and organizations.
Patients
Medical technologies contribute to the wellbeing and health of patients by enabling more accessible and personalized care, precise diagnostics, timely interventions, and convenient self-monitoring methods. These factors accelerate recovery, help detect health conditions faster, and keep people living healthier and longer lives.
Doctors
Healthcare professionals benefit from MedTech through timely and accurate diagnostics that drive informed treatment decisions and ultimately improve patient outcomes. Thanks to automation and machine intelligence, modern solutions free doctors’ time to focus on critical, value-added tasks and developing their skills.
Nursing staff
The advances in technology also make nurses' and carers' lives easier by increasing their efficiency, speeding up routine processes, and facilitating communication. MedTech also reduces the likelihood of human error considerably, e.g., when logging patient information. Altogether, this translates into more patients being seen and better care quality being delivered.
Medical admin staff
Modern technology improves the efficiency of medical office and reception desk personnel, providing easy access to essential documentation, streamlining workflows, and improving communication. MedTech solutions also simplify processes related to insurance claims and reimbursements, making these tasks much easier for the admin staff.
Society and healthcare systems
Entire societies benefit from disruptive technologies through reduced healthcare costs and healthier populations. For any country, medical technology is a highly-profitable, innovative sector that creates a significant number of skilled jobs, serves the economy through exports of goods, and contributes to other industries, like manufacturing.
No innovation comes without its own set of challenges. Breakthroughs in digital healthcare and MedTech are no different. Yet, even though COVID-19 has kicked digitalization in healthcare into high gear, many organizations remain skeptical or apprehensive about updating their care delivery systems and enriching them with MedTech solutions. The reasons behind their fears vary, but we will try to summarize some of their prevailing concerns.
Compliance
Compliance is a recurring theme when it comes to reluctance in adopting disruptive technologies in healthcare. The distribution of any healthcare-related product is associated with a net of complex regulatory requirements and subject to the approval of health regulatory bodies specific to a given country (like the FDA in the USA, EU MDR within the European Union, MHRA in the UK, etc.).
Launching and marketing a product is one thing. Still, as requirements and guidelines keep changing, MedTech device manufacturers and medical software vendors must keep up to date with rapidly evolving regulatory updates.
On top of that, the entire process of product manufacturing or software development must conform to relevant quality management systems and directives. Selecting a knowledgeable technical MedTech advisor to lead the creation and implementation of your digital medicine or MedTech product will help you neutralize risks related to non-compliance and meet the requisite regulations.
Privacy and data security
The collection, processing, storing, and sharing of sensitive patient data is an issue that continues to raise ethical questions in the context of digital healthcare products and medical technology. The issue is substantial, especially as many software systems fail to catch up with the evolving security threats. As HIPAA Journal reports, 2021 was the second-worst year in history in terms of breached healthcare records, with nearly 45 million records exposed or stolen!
With greater freedom and mobility comes a greater risk of exposure. As patients, clinicians, and third-party providers access PII and PHI data via different apps and devices connecting from all corners of the world, ensuring security becomes increasingly challenging. As a result, healthcare software and device vendors must constantly revamp their security to address the new threat vectors. Apart from well-known methods, such as multi-factor authentication, data encryption, anonymization, access rights management, etc., they should always look for new ways of hardening their defenses against all types of cyberattacks.
Processing high data volumes
The massive amounts of health data processed by MedTech devices and digital platforms can also pose a challenge from a technical perspective. The amount of data generated by various medical devices and apps and collected by organizations calls for robust data collection and storage infrastructure. It needs to be well-designed to handle that volume, do it in a compliant and secure way, and enable fast retrieval. Of course, balancing capacity with costs is another issue.
Integrating all the data-generating systems and applications requires a well-designed data strategy and appropriate infrastructure to ensure smooth data flow and sharing. Finally, data isn’t there just to be stored and retrieved. Hospitals and other medical facilities use big data analytics solutions, often strengthened with AI algorithms, to gain valuable insights that inform better diagnosis and treatment decisions. But, again, implementing these systems is complex and involves specialist ICT and data science knowledge. Without it, it may turn out that the investment in an expensive data engine was a waste of time and money.
An effort that will pay off
As significant as they might be, the challenges outlined above should not hinder technological progress and goals set out on an organization's digital health roadmap. Considering the constant advancement in information, communication, and connectivity areas, many of these concerns are being lifted daily, with new solutions and optimizations emerging constantly.
Digital transformation may sound overwhelming, but it's a manageable and worthy endeavor if taken one piece at a time. To make the most of it, we recommend partnering with a trusted team of professionals with experience designing and implementing MedTech products and custom healthcare software solutions. They know how to ensure that the end MedTech or digital health product remains compliant, respects privacy requirements, and guarantees security.
Biggest opportunities for MedTech
Since we’ve covered the shadier side of implementing MedTech and digital healthcare solutions, it’s time for something more optimistic. Let’s start with a handful of statistics. After all, data doesn’t lie.
A quick look at the Fortune 500 list of the world’s most profitable companies will find tens of healthcare-related organizations, with four occupying the top 10 spots. Moreover, health and medical insurance, hospitals, and pharmaceutical wholesaling rank in the top ten of the biggest industries by revenue in the US.
‘But what do they have to do with MedTech?’ you may ask. Think of IoT-based data analytics platforms for insurers, smart medical devices used in hospitals, or medication tracing systems, and you’ll get the answer.
And when you add to that the explosive growth of digital health startups (an eye-popping $57.2 billion in funding last year), the rise in mergers and acquisitions, and a 6,000% growth in telemedicine use due to COVID-19, there’s no denying that digital healthcare and medical technologies are poised to thrive.
In terms of the trends in the development of MedTech devices, we foresee the most significant investments being made in the following areas:
- Data-based diagnostics - Augmenting hardware and devices with data analytics for improved collection, storage, analysis, and data exchange is already happening. We expect this trend to intensify further.
- Nanomedicine - Miniature technologies continue their expansion in medicine. Technology improvements in imaging, diagnosis, and drug delivery, such as a lab-on-a-chip or nanosensors, will move to the forefront.
- 5G-enabled devices - In the next year or two, MedTech companies will be bringing enhanced connectivity to their devices to strengthen the existing healthcare ecosystems and unlock even more powerful data analytics and predictive functions.
- Predictive diagnostics - We believe that soon, medical innovations will allow us to predict certain conditions not only in their early stages but even before they develop. Predictive systems will find their way to commercial wearables like fitness watches and wellness rings.
- Precision medicine - Developing highly individualized and targeted therapies is the ultimate goal of modern medicine, and we believe we’re getting there. This is the future of healthcare.
Building a digital health product: Key requirements
As the demand for medical devices increases, MedTech companies will look to use transformative technologies to enhance their products and develop a distinctive advantage. But regardless of their type and use, all solutions in digital healthcare must meet some basic criteria to stand a chance of hitting it big.
Patient- and clinician-centricity
By their essence, modern medical technology devices empower patients with data and turn them into decision-makers, actively participating in their healthcare. Therefore, patient-centricity is built into MedTech products to deliver personalized treatment. That’s why it’s vital to include patients in every step of designing a MedTech or digital healthcare product, whether it’s EMR software or an artificial eye.
There are many ways to achieve that, from online surveys to inviting a small group of patients to the board meeting to contribute their ideas and provide invaluable feedback. Incorporating patient voices into the development process from an early stage is the best method to avoid losing touch with those who will benefit from your solution.
The same goes for physicians. Although patients are the ultimate beneficiaries of all MedTech solutions, doctors, nurses, and other healthcare professionals are frequently the end-users of your devices and software. Therefore, it’s good to involve them in the product work as early as possible to benefit from their industry knowledge from day one. Doing so will increase the credibility of your product and help validate your engineering team’s ideas.
Tip: Engage patients and doctors in your product development early on, and keep them involved throughout. Consult them during the post-implementation stage, when they can still provide much-needed feedback that will allow you to enhance the next product releases.
Compatibility with future-oriented technologies
Transformative technologies like data analytics, blockchain, or AR and VR are poised to play a huge role in delivering proactive, patient-centric, and timely healthcare services. But embracing change is always a challenge.
Some companies are apprehensive about harnessing innovation in MedTech for fear that the new technology will die down before the investment pays off (remember compact discs, BlackBerry keyboards, and pagers?). On the other hand, early adopters of technologies that do take off take immense advantage of enhanced cost-saving, efficiency, and innovation.
Anyway, none of this matters now. Before, MedTech companies were free to decide whether they were ready to embrace future technologies. But COVID-19 changed everything. The pandemic brought a permanent need for personalized, remote, and flexible healthcare delivery models, and there’s no turning back.
As a result, organizations that want to carry on business as usual have no choice but to transition to the future of health, upgrading business models to incorporate innovation. It’s the only way to continue with strong and differentiated products despite rising patient and provider expectations.
Tip: You’re not alone. To innovate and future-proof your solutions, you can forge partnerships with software companies experienced in delivering technologies underlying medical devices and systems. They will help you overcome barriers to creating a holistic product and stay relevant now and in the future.
Compliance with regulations
As data processing and connectivity become integral to healthcare solutions, new regulations emerge to protect the identities of patients and providers and safeguard the storage and sharing of their data. Keeping abreast of all of them, while mandatory, is tough. And not only because the regulations concerning the sale and distribution of medical device products and systems are specific for each country.
Another significant challenge is that regulatory developments are still advancing, so it takes effort to catch up with all the changes and updates. Besides, the complexity and number of essential certifications and approvals increase with the technological sophistication of a given device or software application.
For example, regulatory bodies in some countries are extending their oversight to the developers working on medical device solutions. In addition, other regulations exist to monitor artificial intelligence and machine learning in healthcare products. For example, the European Union directives impose requirements on software providers, including the obligation to observe quality management procedures and draw up technical documentation, or deliver specific information, such as user manuals supplied with the device.
On top of the strict requirements related to medical technology, MedTech manufacturers must comply with regulations around creating and publishing software. Most of them are associated with data encryption, ensuring appropriate access controls, and monitoring and reducing security threats. However, additional guidelines and laws may exist depending on a specific product, such as compliance with Payment Card Industry Data Standards.
Tip: Failure to observe regulatory compliance requirements can lead to penalties, fines, and even a ban on marketing your product. Therefore, you must ensure proper planning and implementation of features and updates that will allow your products to fulfill regulatory obligations. Again, liaising with an established partner who has experience with the development of MedTech solutions can make it easier to manage the complexity of medical device regulatory changes.
Where to find and how to hire MedTech developers
Let’s say you plan to build a brand-new MedTech product. Whether you want to launch an advanced medical device powered by big data analytics and AI, create an EHR tool, or produce a mobile app for tracking heart rate, you’ll need software.
One of the first things you need to do is assemble a team of reliable healthcare software engineers who will help you create the software underlying your solution. But it might be easier said than done because skilled healthcare software developers are generally in short supply. Finding professionals with a background or experience in healthcare projects is twice the challenge.
According to extensive research by Korn Ferry, by 2030, more than 85 million jobs globally could go unfulfilled, and technology will be among the industries most affected by the shortage. Already now, nearly two-thirds of companies lack the skills required to carry out their digital transformation plans. As the break-neck speed of technological innovation continues and more areas requiring software knowledge abound, the demand for tech talent is likely to surge.
Savvy organizations with their eyes set on progress and success employ different tactics to fill in technology vacancies and build digital healthcare products. We’ll briefly review some of them and advise you on the essential skills to look for in MedTech software developers and custom healthcare software development companies.
What hiring options do you have?
There are several approaches to retaining a specialist in healthcare software development services. We won’t mention freelancers, as they are usually more suitable for handling individual tasks or supporting smaller projects in the short term.
Building an in-house healthcare software development team
Some companies prefer to invest in an in-house software development team or map the required roles and develop careers within their workforce to fill them in the future. However, despite the obvious benefits of this strategy, such as adherence to company culture, seamless collaboration, or the flexibility to make real-time adjustments, using in-house staff does not work for many businesses, especially small and medium-sized.
The greatest challenge consists of finding qualified employees with the right skill set, considering the limited talent pool in software development. Research on this topic varies, but generally, it takes up to three months to retain a new hire. Then, one of the most notable disadvantages of in-house teams is the high cost of retainment, onboarding, and maintenance.
When you factor in expenses such as equipment, training, sick days, holidays, benefits, taxes, etc., costs add up quickly. And there’s no guarantee that this investment will pay off. Considering the high turnover in the IT market, your new hire may wave ‘goodbye’ right when the project is about to start.
Using an outsourcing company
By ‘outsourcing company,’ we mean international outsourcing giants like Wipro, Infosys, or HCL and smaller companies providing body-leasing services. On the one hand, using their healthcare software development services allows you to quickly retain the required skills to get the project going fast. Besides, you can choose the best service model for your needs and budget, easily scale up and down the outsourced team, and save on HR and equipment costs.
On the other hand, there are many traps when using an outsourcing contractor. What sometimes looks like a deal of the lifetime may lead to low-quality work, impacting your profitability. Besides, be mindful that outsourcing contracts require you to give up some control over your project. You must develop clear and effective lines of cooperation to have your say on the direction your project is heading and address issues regularly, not once the entire code repository is complete.
Additionally, when sourcing specialists from distant overseas locations, make sure that there’s some time zone overlap and verify all specialists' level of English fluency. More importantly, ensure your outsourced team understands and subscribes to your company culture, values, and quality standards.
Tech talent marketplace with pre-vetted experts
Here’s another widespread solution, particularly recommended for projects that demand domain expertise paired with business acumen. To find the right people providing high-quality healthcare software services, you can use marketplaces for on-demand, pre-vetted software development contractors and consultants. Examples of such platforms and agencies include Toptal, Guru, Fiverr, and us—Ideamotive.
Depending on the provider, these marketplaces either simply act as a point of contact between companies and freelancers (PeoplePerHour, UpWork, Fiverr), or expert agencies that apply a rigorous vetting process to assess each professional’s skills, background, MedTech industry expertise, personality, and business acumen.
Engaging with this type of provider entails many benefits— the high quality of the services provided being the major one. In addition, talent marketplaces have access to a unique, verified expert pool comprising hundreds of experienced specialists, which radically shortens your recruitment process.
The available specialists are experts in particular areas, like web development, backend programming, UX design, software architecture, and technologies (specific programming languages and frameworks, blockchain, AI, IoT programming, etc.). Moreover, they’ve got years of experience working with different clients, which translates to ultra-short onboarding and a business perspective on software projects. Usually, such platforms and marketplaces offer contracts of any duration, from small assignments to huge collaborations spanning months and years, if needed.
Are you tired of using Fiverr to find the best talent?
Check out this blog post on the best Fiverr alternatives and see where to go instead.
[Best Fiverr Alternatives For Hiring Developers]
Essential skills for a healthcare software engineer
No matter what approach you adopt to hiring MedTech software developers, there are certain skills that all quality professionals should demonstrate. But before we share them, remember that the rate shouldn’t be the primary factor underlying your decision to hire.
The IT industry is indeed notorious for charging exorbitant fees. However, a quote that seems too cheap is a definite red flag. The cost of poor quality may be higher than you think. When the price seems too good to be true, it likely is. Remember: “The bitterness of poor quality remains long after the sweetness of low price is forgotten.”
Fortunately, there’s plenty of choice between excessive and suspiciously cheap rates for professional software development services. So search within that range, and take a close look at other essential qualities of a software expert (or an entire team) to build your digital medicine product.
A proven track record in MedTech and digital medicine development
Digital healthcare products need to comply with different security and availability standards. They may also involve the use of MedTech industry-specific frameworks and APIs. This is the knowledge that every healthcare developer should possess to produce high-quality and compliant code.
Among others, MedTech professionals specializing in software for the healthcare industry should be familiar with:
- Healthcare revenue cycle workflow, comprising elements such as compliance with health and financial regulations, collection, storage, and transfer of sensitive data, or details related to claims and reimbursement, billing schedules, or payment models.
- Integration standards and frameworks. No healthcare application or platform can be approved without meeting the requisite standards for integration. They include SCRIPT, DICOM, ANSI X12n, and several others. The same goes for the knowledge of integration frameworks used specifically in MedTech software.
And this is, of course, on tops of more general skills and capabilities, such as the knowledge of specific programming languages, frameworks, libraries, the understanding of quality assurance and testing tools and metrics, key methodologies for efficient code implementation, and the ability to integrate the software with third-party solutions via APIs.
We can see that a developer or a team of specialists with experience in MedTech have an advantage over professionals who have never engaged with healthcare software development services. And it’s your responsibility to verify their background. How? You can, for example, check out a person’s or company’s LinkedIn page, go through reviews on Clutch or another ranking portal, or ask for referrals and examples of past projects.
Other software-related roles that you might need
When building a MedTech software product, it’s not enough to get someone who knows how to code. Depending on your project, you might need particular skills and experience tied to programming expertise and look specifically for:
- mHealth developers — Mobile health developers will be essential if you want to build a mobile healthcare app or integrate the existing web-based system onto mobiles. Typically, they will be working with one or more programming languages: Kotlin, Swift, Rust, R, Python, Java, or React.
- IoT developers — Like mHealth developers, IoT programmers have their field of specialization. Namely, they write code that underlies and connects smart sensors and devices. A qualified specialist should be able to program and know how to test and document IoT solutions and integrate them with third-party systems and devices.
- AR/VR developers — C#, C/C++, Java, JavaScript, and Python are among the most popular languages behind augmented, mixed, and virtual reality software. Therefore, if you’re looking to launch such an application, look for professionals fluent in these technologies. Apart from them, VR and AR developers should possess some skills in video editing, computer-aided design, and 3D modeling.
- Data and machine learning engineers — While AI, ML, and data science are huge topics, generally speaking, all teams developing modern healthcare software must include at least one expert in data analytics, machine intelligence, or both. The applications of these techniques are numerous (click here for more details). Still, on the whole, they serve to provide automation and optimization of systems and processes in healthcare organizations and improve patient outcomes by processing and analyzing massive datasets in seconds.
- Blockchain developer — As the number of applications for distributed ledgers in healthcare apps is growing, blockchain developers are applying their skills to build MedTech products. To do that, they should be well-versed in the principle of blockchain architectures and familiar with concepts of cryptography, smart contracts, distributed ledgers, and other related terms.
04 Top MedTech players
Up to 80 percent of startups ultimately fail. Unfortunately, MedTech startups are no different. Actually, it might be even harder for them to succeed, as they’re in an incredibly competitive and difficult industry.
However, to pick up your spirits, there was never a better time to try one’s hand at launching a profitable MedTech product. 2021 was another record year for digital medicine and MedTech startups, which raised $29.1 billion. In comparison with the year before, investment in the market nearly doubled. And the perspectives for 2022 and beyond are likely to be bright, as telemedicine has blossomed in the pandemic times.
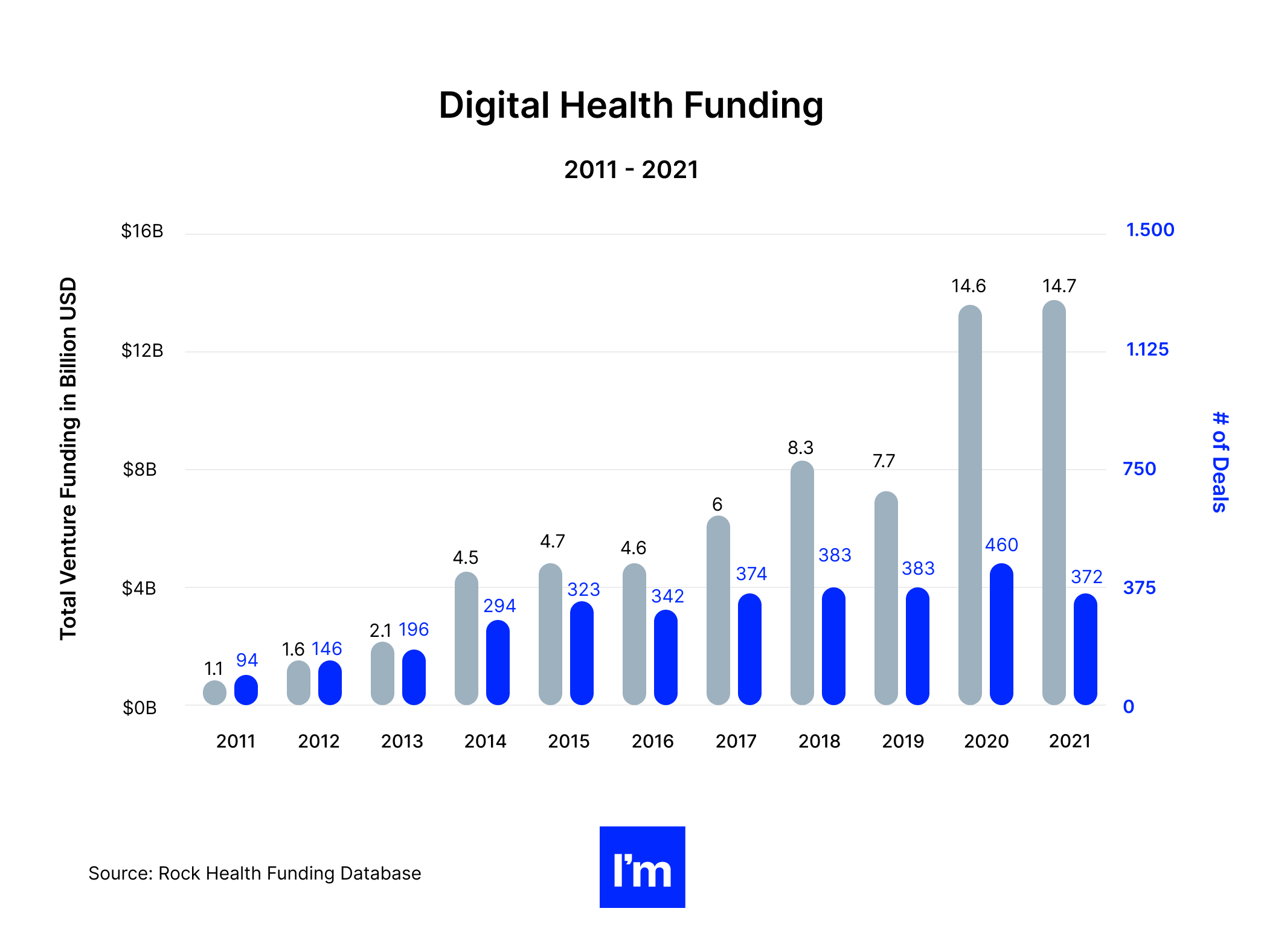
Powered by the colossal use of virtual care services, new payment models and programs, and the maturing of enabling technologies like IoT, blockchain, or AI, digital health solutions stand a huge chance of succeeding. While launching a profitable app or software system is never easy, momentum is building around MedTech devices and software. Hundreds of success stories from healthcare tech startups provide proof that nothing is impossible in this field, provided you have an ingenious idea and top it up with flawless execution.
MedTech startup unicorns
As of 2021, there were 76 MedTech startup unicorns worldwide. Many of them joined the list last year, proving that the sector is continuing to gather momentum, and that hitting the jackpot in MedTech is possible.
“We’re seeing an increase in round sizes, new investors, and the pace of digital health funding. There’s an acceleration of exits and the emergence of combined companies that can address health care more broadly,”
said Michael Pimental, partner, and co-founder of CVS Health Ventures, summarizing the explosive growth in digital health investments over the last two years. Numbers back his statement.
Namely, the monthly funding for digital health initiatives in June 2021 was almost triple compared to June 2020. Additionally, the first half of 2021 was the period with the largest funding activity in the American digital health market ever. The areas with the biggest funding include mental health, fitness and wellness, on-demand healthcare, and R&D.
That is not to say pursuing MedTech investments and profit is easy. On the contrary, it takes a lot of creativity, instinct, knowledge, and determination to succeed. Therefore, among those lucky companies that made it to a $1 billion valuation, we will find groundbreaking products and apps that stand out from the crowd and truly make a difference.
Let’s take Komodo Health, for example. The computer software company brings market intelligence to healthcare and life sciences, creating a map that compiles massive amounts of healthcare data. By applying data science, the company hopes to help payers and companies identify gaps in care and improve their services.
Ginger, another massively successful startup, provides the technology underlying on-demand mental health support by licensed therapists and doctors. In 2021, the company announced its plans to merge with another popular wellness and mental health platform, Headspace.
On the unicorn list, we can also find Grail. The company is pioneering a multi-cancer detection test that can detect over 50 cancer types, most of which are not efficiently screened today.
If you’re more into robotics, CMR Surgical may interest you. The founders of this British technology company created a robotic surgery system that assists surgeons, ensuring enhanced precision and control.
And if your company lacks a surgical or medical background, why not explore some ideas within a broader category of healthcare, fitness, and wellness? Like Zwift, for instance, an app for indoor cycling for professionals and amateurs. The company joined the unicorn league in 2020, scooping an eye-popping$450 million in the last funding round.
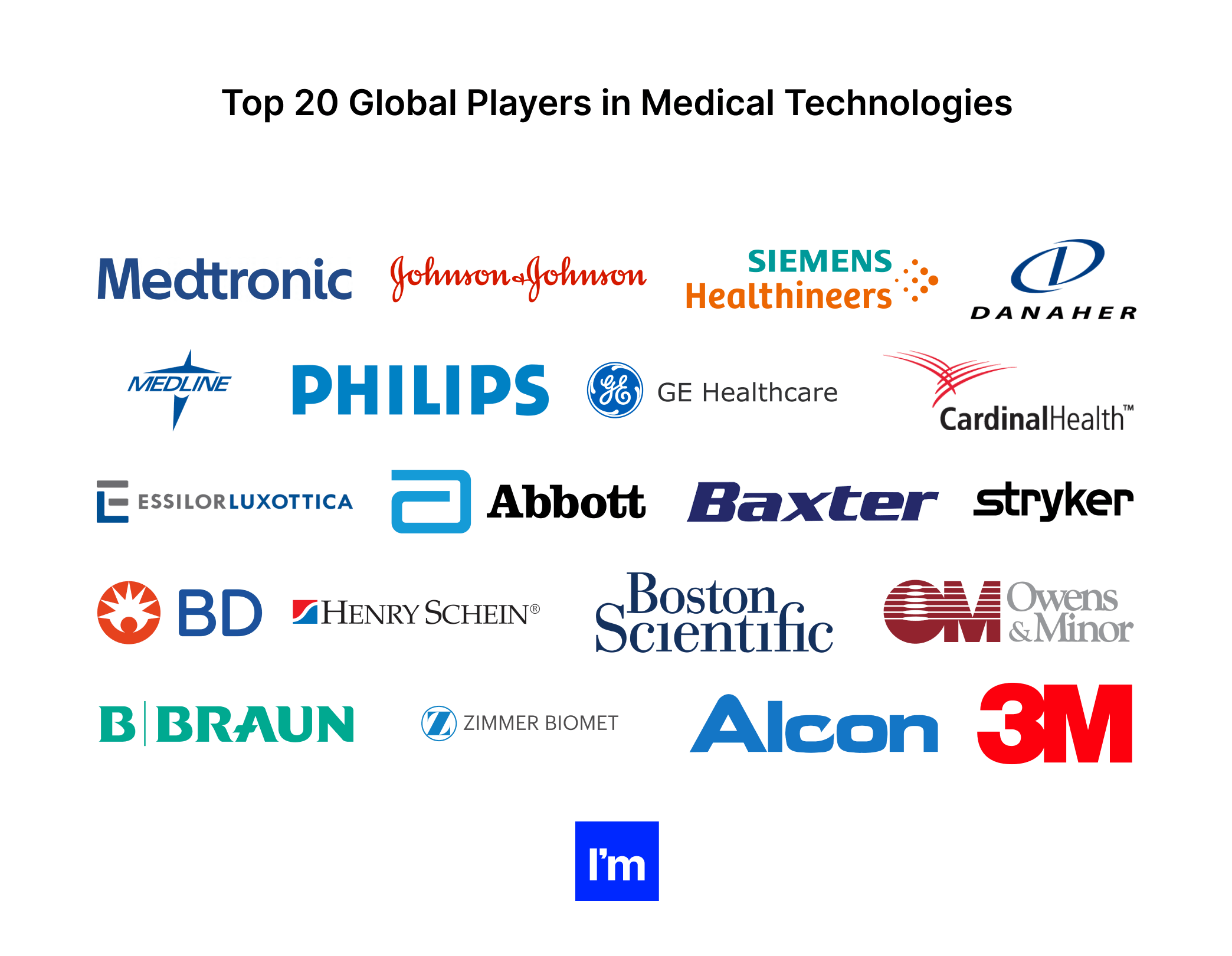
Of course, it’s not just startups that use the opportunities created by MedTech to make a profit while helping people at the same time. Some of the world’s most renowned corporations also invest in the market, building hardware and software solutions that power modern healthcare.
To find out who’s leading today’s MedTech solutions, check out this rundown of 20 medical technology companies generating the highest revenues (go here for the full list). You might recognize some of them (like Siemens, for example) from other industries, not even realizing they are nibbling on the massive healthcare applications market cake worth $74.2 billion in 2020.
- Medtronic - This American-Irish leader in medical technology started as a repair shop for medical equipment. Today, the company is well-known for its robotic surgical platform, orthopedic implants, insulin pumps, and many more innovative MedTech devices. It also delivers integrated health software solutions. In 2021, its revenues exceeded $30 billion.
- Johnson & Johnson (medical device segment) - Nowadays associated primarily with its COVID-19 vaccine, J&J is one of the world’s largest conglomerates in the medical devices segment. Under different subsidiaries, the company manufactures surgical and orthopedic technologies, electrophysiology tools, breast implants, eye protection and treatment products, and many more.
- Siemens Healthineers - With over $20.5 billion in revenue generated last year, the German company takes the third spot on the list. Its comprehensive portfolio includes devices and healthcare solutions along the entire care continuum. Siemens Healthineers also develops a range of digital healthcare solutions, including magnetic resonance imaging, radiation therapy software, VR and 3D imaging software, and workflow solutions.
- Philips - You may associate Philips with TV sets or light bulbs, but its subsidiary, Royal Philips, is one of the biggest leaders in medical technologies. It is well-known for imaging systems and diagnostic products and invests big in biotelemetry and AI-based solutions for cardiac diagnostics.
- Danaher (life sciences and diagnostics segments) - A Fortune 500 science and technology innovator based in Washington D.C, Danaher offers medical devices and analytical instruments for lab and scientific research.
- Medline Industries - Medline manufactures and distributes healthcare supplies ranging from wheelchairs and surgical supplies to face masks. Considering the soaring demand for gloves, masks, and other protective equipment following the COVID-19 outbreak, it’s only logical that the company is in the top 10 of the world’s most profitable businesses in healthcare.
- GE Healthcare - Like Siemens or Philips, General Electric also has its healthcare subsidiary providing a wide array of medical technologies, digital infrastructure, data analytics, and decision support tools used by medical professionals and companies.
- Cardinal Health (medical segment) - One of the US’s top-earning businesses, Cardinal Health distributes and manufactures pharmaceuticals and medical and laboratory products. The company also invests in its technology department, providing performance and data solutions for hospitals and other healthcare facilities.
- EssilorLuxottica - This French-Italian conglomerate is probably one of the few top-grossing healthcare solutions providers focusing solely on one niche—eyewear and eye vision solutions. It designs and manufactures ophthalmic lenses, optical equipment, and glasses. In 2020, the company launched a digital marketing tool, EssilorLuxottica 360, which helps practices target prospective patients, raise visibility, and capture in-store sales.
- Stryker - Stryker originally delivered innovation in the orthopedic sector, but today, its solutions also include other specialties, like neurosurgical, spine, endoscopy, emergency care, or sports medicine. The company provides numerous software types, from hospital enterprise software and a data review platform to a surgical reporting suite.
- Abbott (medical device segment) - The company comes from a pharmaceutical background. It manufactured its breakthrough synthetic antiseptic, Chlorazene, in 1916. With time, it has expanded to embrace such areas as devices supporting the treatment of heart diseases and conditions, chronic pain, and spinal cord dysfunctions. Among the company’s products, we will find a dialysis device equipped with a remote patient monitoring platform. Abbott was also one of the first to launch a rapid at-home COVID-19 test kit.
- Baxter - Baxter mainly produces and sells products to treat chronic and acute conditions, including kidney disease, trauma, hemophilia, and immune disorders.
- Henry Schein - Yet another distributor on the list, Henry Schein specialized in distributing medical and dental supplies, pharmaceuticals, and vaccines. However, it also provides a wide array of software for the healthcare industry, including EHR systems, solutions for dental practices, healthcare financial software, and patient communication solutions.
- Boston Scientific - Boston Scientific leads the way in interventional cardiology, endoscopy, urology, and other specialties, designing and producing cutting-edge medical devices and the accompanying software. More recently, the company increased its investment in remote patient monitoring solutions.
- Becton, Dickinson (medical segment) - For Beckton, Dickinson, or BD, it all started with a glass syringe. Today, the company still sells syringes and hypodermic needles while also manufacturing infusion systems, diagnostic and surgical products, and other medical devices and technologies across three segments. In addition, BD also implements a range of software solutions such as clinical monitoring and notification tools, digital knowledge portals, infection surveillance systems, pharmacy intervention and documentation software, and many others.
- Owens & Minor - This is a logistics company specializing in pharmaceuticals, wholesaling, and distributing personal protective equipment, IV start kits, skincare products, and other supplies. It also offers a digital inventory management solution for clinicians and hospitals.
- B. Braun Melsungen - It began by selling herbs. Now, the company spans over 60 countries, offering products for infusion therapy and pain management, IV therapy products and solutions, and drug delivery systems. One of its subsidiaries also manufactures surgical equipment and power systems.
- 3M Co. (healthcare segment) - The medical division of a multinational conglomerate develops therapeutics and vaccines, food safety indicators, skin, wound care and infection products, filtration and purification systems, among others. As a technology company, 3M is also one of the largest software providers for healthcare, creating solutions spanning from reimbursement platforms to medical coding software.
- ZimmerBiomet - A publicly traded medical device company, ZimmerBiomet focuses on orthopedic reconstructive products, sports medicine, trauma solutions, dental implants, and surgical devices. It has also launched a software platform for collecting and sharing IoT data between smart implants, apps, and surgical systems. Last year, the company launched a revolutionary smart knee implant.
- Alcon - Last but not least, Alcon was a subsidiary of Novartis, another big name in the MedTech business. Today, the company’s offering includes surgical and vision care products. Alcon also provides refractive technology solutions.
Big tech’s investments in digital healthcare solutions
If we look at the world’s most profitable and influential healthcare software vendors, we’ll find names such as Microsoft, Oracle, SAP, Epic Systems, and even Salesforce topping the list! The scope and variety of MedTech services and digital health solutions these companies provide are unending.
 For example, Microsoft is investing big in healthcare. Some time ago, the company launched Microsoft Cloud for Healthcare, a dedicated cloud to manage health data at scale and securely and underlie solutions enabling teleconsultations. The company is also pursuing opportunities related to mixed reality with its HoloLens 2 device, and AI—empowering healthcare organizations to deploy an intelligent virtual health assistant using Azure Health Bot.
For example, Microsoft is investing big in healthcare. Some time ago, the company launched Microsoft Cloud for Healthcare, a dedicated cloud to manage health data at scale and securely and underlie solutions enabling teleconsultations. The company is also pursuing opportunities related to mixed reality with its HoloLens 2 device, and AI—empowering healthcare organizations to deploy an intelligent virtual health assistant using Azure Health Bot.

Amazon is also launching its healthcare business, Amazon Care, enabling employers to provide their teams with access to high-quality medical care within minutes via a digital health platform.

Google is another active investor in the MedTech and digital healthcare market, pumping its money into startups dealing with precision medicine, virus prevention, gene editing, etc. Apart from that, the company has its Cloud Healthcare API that allows standardized data exchange between healthcare apps using Google Cloud.

SAP delivers an entire suite of healthcare-focused software products. From patient engagement platforms, diagnostics systems, health data insights, and digital billing tools, to healthcare financial software.

And if you were wondering about the implementations of Salesforce in healthcare, the company supports medical professionals and organizations with a healthcare CRM software platform that provides a 360-degree view of each patient’s health journey for a better experience.
05 Wrapping up: The future of MedTech
In early 2019, the WHO released the first guidelines on digital health interventions. It comprised recommendations on using digital tools to enhance healthcare delivery for patients. The release had been planned for two years in response to healthcare vendors' and providers' increasing adoption of modern technologies. It was intended to incentivize health systems and organizations to improve the uptake of digital health solutions. Considering the events that followed barely a few months after the publication, the timing was perfect.
It was already evident that global healthcare delivery needed a major overhaul at that time. The guidelines set a milestone for global health systems, providing clear evidence that digital tools directly impact the strengthening of health systems worldwide. And what is the state of these proposed changes? Or, more importantly, what does the future hold for digital health and MedTech?
We don’t have a crystal ball, but it doesn’t take clairvoyant powers to make some pretty reliable predictions about the direction in which MedTech will develop in the next few years. First, let’s have a look at some numbers.
MedTech industry is growing strong, and so is the competition
Between 2021 and 2025, the global AI in healthcare market is predicted to progress at a record-breaking CAGR of 35.59 percent. Analysts believe that it will hit a value of $22.68 billion at the end of that period. The healthcare big analytics market will also continue to exhibit strong CAGR growth of 12.5 percent between 2021 and 2026. Additionally, analysts predict that MedTech stocks are poised for major growth, and health-tech funding shattered yearly records in 2021.
All this data indicates that even though the pandemic has challenged healthcare systems globally, it has also given MedTech an impetus for growth. Indeed, digital health solutions and smart devices continue to play a vital role in warding off the virus and transitioning to the new, enhanced format of medical care.
Teletherapeutics, symptom self-checker apps, home testing kits, and even drones are used to enforce lockdowns and detect people with fever—just a few years ago, these technologies mostly belonged to the world of Hollywood pandemic sci-fi thrillers. Today, they are an integral part of healthcare delivery globally.
"Harnessing the power of digital technologies is essential for achieving universal health coverage."
Dr. Tedros Adhanom Ghebreyesus, WHO's Director-General
COVID-19 created new demands and new challenges
The pandemic has acted as a catalyst for adopting novel MedTech devices and software solutions because it has left no other choice. With traditional healthcare services strained, patients had to get a crash course in eHealth technologies, while medical organizations scaled up their investments in digital, AI, and data solutions overnight.
As we’ve entered the third year of the global crisis, the uptake in digital health solutions and innovative technologies will continue for the long haul. After all, when different age groups are already familiar with and used to a certain level of health delivery, it’s unlikely they’ll be willing to revert to the old ways of doing things once the pandemic ends.
To take advantage of these favorable circumstances to protect and expand market share, MedTech organizations should follow several principles when reevaluating their business models and value proposition:
- Develop a better understanding of the end-user. As the reality of healthcare delivery has changed, so did MedTech beneficiaries and consumers. Patients are now actively participating in their healthcare, while medical professionals learn how to improve their services by embracing data and digital tech.
- Build AI and analytics skills. Healthcare providers take vigorous steps to adopt data-driven solutions, providing a holistic view of each patient and unlocking faster and less costly treatment. As medical devices become increasingly connected, big data is the leading technology powering MedTech solutions today.
- Embrace omnichannel engagements with patients and users. Developing a breakthrough solution is one pillar of success for MedTech companies, successfully marketing it to the target audience is another. To support and strengthen remote interactions with their target buyers, MedTechs have no choice but to embrace omnichannel. A vast majority of them already leverage multiple channels (in 2020, 82 percent of US MedTech and 76 percent of European launched their product on social media, and 79 and 78 percent respectively via email), but the trick is to merge the presence on all of them into one seamless, frictionless user experience.
- Partner with technology consultants. It takes diverse skills and expertise to deliver modern medical device solutions and software systems end-to-end. New roles such as data analyst, systems engineer, UX specialist, IoT developer, etc., have emerged, all of which are an integral part of today’s cross-functional MedTech teams. However, unless your company is a multinational conglomerate, it’s unlikely that you have the resources to fill in all these roles and capabilities. Partnering with a trusted MedTech advisor with experience in developing technology solutions AND bringing them to the market will make creating a winning MedTech product much easier.
COVID-19 has presented a unique opportunity for healthcare technology providers to rethink and reform their products, strategies, and operating models, but now the ball is in their court. While keeping a tight grip on the budget and seeking cost savings never go out of fashion, a more nuanced approach is essential for MedTechs to thrive in the future; one focused on user-centric product design, remote healthcare delivery, and innovation, especially around data analytics and artificial intelligence software.
And now, really, is the last call to embrace this approach and ride the digitization trend. Latecomers and laggards may be heading for disaster, failing to catch up with those ahead. On the contrary, tomorrow’s MedTech leaders will confidently seize a considerable market share by acting now to intertwine advanced technology and business strategy.
As we look towards the future, it's clear that technology will continue to be an essential player in the evolution of healthcare. The emergence of EHR software like MEDITECH and the proliferation of digital health solutions will be instrumental in the transformation of MedTech.
Emerging healthcare software, from EHR systems to medical device compliance software, is streamlining the management of health information while bolstering data security. MEDITECH's EHR software, for instance, is reshaping how medical records are handled, contributing significantly to the effectiveness and efficiency of care delivery.
The rise of regulatory affairs software and regulatory management software is another trend to watch. These technological solutions automate and simplify compliance processes, which is particularly crucial in the strictly regulated healthcare sector. Software solutions like Rimsys Regulatory Management Software are ensuring compliance, reducing complexity, and improving overall operational efficiency.
Moreover, the incorporation of quality management software for medical devices, like Greenlight Guru software, is taking device manufacturing to the next level. By ensuring quality control and regulatory compliance, these systems are making medical devices safer and more reliable.
Furthermore, the growing reliance on health information technology software indicates a shift towards more integrated, data-driven healthcare. The use of health system software is becoming increasingly common in hospitals, aiding in everything from patient scheduling to billing.
Lastly, with the advent of innovative hospital software, the management and operations of medical institutions are set to become increasingly seamless. Software solutions like MEDITECH accounting software are already changing how hospital finances are managed, leading to more efficient resource allocation.
In essence, the future of MedTech lies in harnessing these technologies to revolutionize healthcare, making it more patient-centric, efficient, and inclusive. The innovations we're witnessing today are just the beginning of a much larger transformation.
Ready to build your MedTech product?
We run a vast network of vetted software development professionals, including MedTech experts. We can provide you with technical consultancy, add devs to your existing team or assemble one from scratch.
Rated 4.8 / 5.0 by clients from various industries and locations.

